Professor Christopher Whitty presents a series of lectures on infectious diseases, demonstrating how they have dominated medicine and mortality in the UK. Infectious diseases remain a major threat, and the combination of widespread travel, antimicrobial resistance to drugs and a rising proportion of the population in older age groups means that the threat is now increasing again.
Some infections come in repeated epidemic waves, others are new to human populations. A known human threat such as influenza may mutate, or a new infection jumps the species barrier from animals to humans: recent examples include HIV and Ebola, and the historical example of plague. What happens depends on the route of transmission. Our methods for tacking an airborne disease like influenza are different from those for touch (Ebola), insect vector (Zika), water (cholera) or sexual transmission (HIV).
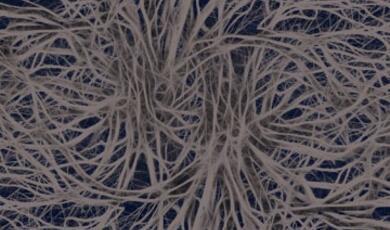
The brain is well protected against most infections, but once they get into or around the brain they can cause fatal or serious long-term consequences. Some infections are well adapted to the brain including meningococcal meningitis. Control measures including vaccination have reduced the risk of some, but not all, of these very serious infections. Professor Whitty looks at how infections get into the brain, their effect and how we can prevent and treat them.
Certain infections have a specific impact on the peripheral nerves. Some are predominately on the motor nerves causing weakness or paralysis (for example polio). Others affect the sensory nerves. Some bacteria produce toxins which damage nerves function including tetanus and diphtheria.
The lung has a large surface area, is open to the outside world and is the site for common serious infections, in particular pneumonia. The heart is less susceptible to infection, but heart infections can be severe. Some lung infections are becoming less common due to vaccination, whilst others are likely to increase globally. Infections via the respiratory route are often the most difficult to combat via public health measures.
Our gut is permanently full of large numbers of bacteria, but serious infections rarely occur due to its extraordinary immune system. Specialised bacteria and parasites can, however, damage the gut or its functions. The liver can be damaged by hepatitis viruses, parasites and other infections. Common gut bacteria which normally cause no serious problems can bypass the gut's defences and cause serious infections including septicaemia. Public health has reduced but not eliminated transmission of these potentially dangerous infections.
The very young and the very elderly are particularly susceptible to infections. Some infections caught as a child are usually trivial but are likely to be much more severe in adults, or present differently in different age groups. Otherwise minor infections can have major effects in pregnant women or particularly on their unborn babies such as rubella and Zika. The changing pattern of disease as we progress in life has implications for treatment and prevention.


 Login
Login