The Origins of the NHS
Share
- Details
- Transcript
- Audio
- Downloads
- Extra Reading
This lecture looks at the origins of the NHS; there have been many historical debates about the NHS and its origins. Such questions which are discussed are the debate about conflict or consensus. Did the NHS come about through consensus - or did it have to be fought for?
Part of the Safeguarding London's Health, Monday's at One lecture series.
Other lectures in this series are:
Medieval Hospitals of London, by William Ayliffe FRCS PhD
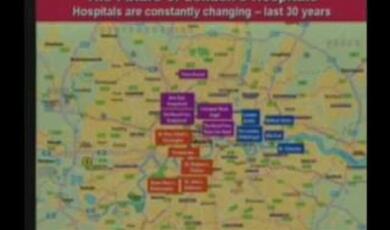
London's Hospitals Today, by Geoffrey Rivett
The Future of London's Hospitals, by Dr Patricia Oakley
Download Transcript
SAFEGUARDING LONDON'S HEALTH - THE ORIGINS OF THE NATIONAL HEALTH SERVICE
Professor Virginia Berridge
Slide 1
I'm going to start with a slide of the NHS as it is now. This seems a long way from 1948 and the many changes of organization have occurred over the last 60 years. I don't want you to look at this in too much detail but just bear in mind two things- the role of parliament at the top and of the Minister of Health right at the top. We can also see the organization is fragmented .This links to some of the themes I want to draw out in the lecture today.
Slide 2
I am going to start with the paradox of the NHS-why it took the form it did:
Why did Britain, with a strong tradition of insurance funded health care, and of health services funded in local government, adopt a tax funded system for the NHS based on the hospital sector and centrally directed.
There were two other models of health care in terms of organization and funding already in operation in pre war Britain-why were these not chosen as the basis for the new service? This is not just an academic question- because the choices made in 1948 affected the choices made by politicians ever since.
Slide 3
This is what I'm going to talk about in the lecture. The plan of the lecture is this. (See slide)
1. The paradox of the NHS
2. The origins of the NHS: more distant and immediate
3. The successes and deficiencies of the NHS
4. Issues for the present.
Slide 4
A basic listing of some key dates to clarify what happened when. I will refer to most in the lecture:
- 1911 National Health Insurance
- 1919 Ministry of Health
- 1920 Dawson Report plans universal system
- 1929 End of the Poor Law
- 1937 Political and Economic Planning Report
- 1939 Emergency Medical Service
- 1942 Beveridge Report
- 1944 Coalition White Paper
- 1945 Labour Government elected
- 1946 NHS Act
- 5 July 1948 'The appointed day'.
Slide 5
Let's go back well before the NHS and start by looking at some early precedents in terms of funding and organising health care.
Firstly health insurance which I mentioned just now. How did this operate?
Respectable working men would be accustomed to join a friendly society in the nineteenth century. Even in 1815 these covered over 8 % of the population. These offered a variety of benefits according to level of contribution and this included sickness benefit. The Hampshire General Friendly Society is shown on the slide- these offered payment if you were ill and some access to medical care. These sorts of societies would employ their own doctors- this was known as club practice. So doctors were under lay control in this system. If you know the novel The Citadelby AJ Cronin, in it there is an unsympathetic portrait of club practice.
Then came the Liberal government at the turn of the twentieth century with Lloyd George's welfare reforms .These are on the slide- school medical inspection, old age pensions, which have their centenary this year and unemployment insurance. These came about because politicians and others were afraid of the 'future of the race' - the fear of imperial decline because of the Boer War. They also looked at previous developments in Germany under Bismarck.
These reforms were followed in 1911 by national health insurance which provided a system part paid by employees part by employers and part by the state. It gave wage replacement for illness and gave the panel system for GPs. So it widened the sort of coverage people had had under friendly societies and extended it to all wage earners.
Slide 6
This insurance based system developed in the interwar years. But it was limited as you can see from the slide. Lots of people were excluded-women if they were not wage earners, young people under sixteen and the elderly who were economically inactive.
It was also under financial strain-friendly societies went out of business and the approved societies made moves to pool their resources.
But it's also important to remember that it was not at all popular.
Panel patients resented their unequal status and there was widespread demand for better access to hospital treatment (which was not covered except for TB) and for better treatment of dependents. Earlier on many working class people had been hostile to the idea of state welfare at all- they wanted to provide for themselves through the Friendly Society system.
Doctors also disliked the system-GPs because of restrictions from the approved societies (which was like club practice) and specialists because of the impending bankruptcy of the voluntary hospitals.
It's important to remember also that other systems operated- there was widespread use of self medication and remedies were bought over the counter from the pharmacist- this is illustrated in this slide picture.
Let us now turn to what was happening in the hospital system.
Slide 7
The voluntary hospitals first-there were 1,000 of these ranging from the very small to the prestigious teaching hospitals. The side shows you UCH in London but there were others such as Barts, the subject of the lecture last week.
The majority were facing severe financial problems by the inter war years. The original system of charitable donations and free entry was breaking down. They were admitting paying patients and people were supporting them through hospital charities and contributory schemes. The hospitals were also mislocated and could not satisfy rising demand.
Another hospital system was run by local government, who had taken on the Poor Law hospitals after the PL came to an end in 1929.
Some of these hospitals were then developed into a municipal hospital system- the best example of which was in London. The LCC hospital system under Herbert Morrison had 70,000 beds and was one of the largest systems in the world.
But this was not the case in all areas-as Martin Gorsky's work on SW England has shown, some hospitals and infirmaries remained under the aegis of the local public assistance committees and these were mainly the long term care institutions catering for the chronic sick, elderly and the mentally ill. These were not improved and had poor quality and stigma. You can see this in the pictures here- people waiting for admission to a ward and the prison like structure of the Poor Law buildings. In this relationship we can see some of the origins of current problems with health and social care.
Slide 8
This brings us to the other aspect of the pre NHS health system-health services based in local government and run by the local public health director, the Medical Officer of Health (MoH). The MoH would be a well known local figure in many areas- I can remember even in the 1950s the MoH in Windsor, my home town, Dr McClatchey giving me my polio sugar lump in the Town Hall, Kipling Buildings. The picture at the bottom of the slide shows this relationship-you contacted the MoH if there was something wrong with your milk.
In the 1930s the MoH was running a huge empire and this seemed to many to be a proto state service- in fact this sort of discussion round public health had been going on since the late C19th. Look at the top slide and you can see some of the services this system covered.
The operation of this system pre war has attracted extensive and ongoing historical debate, in part because its relevant to some of the issues that have come back on the agenda for today.
Some historians , most notably official historian of the NHS Charles Webster and Jane Lewis at LSE, have criticized the service for its conservatism and lack of responsiveness .Webster argued that MoHs did little about poverty and malnutrition and Lewis argued that they were slow by comparison with other countries to adopt new preventive techniques such as diphtheria immunization. So their assessment of public health is not a positive one.
Recently however other historians' work has placed public health in a better light. Historians Alysa Levine, John Stewart and Martin Powell have examined the spending patterns of public health departments and have found that many were showing increased spending in the 1930s.Real choices about health care could be made at the local level.(again there is contemporary relevance for this)
But the role of the MoH at the local level remained controversial-there was for example conflict with the GP over the same territory (If you have read AJ Cronin's Dr Finlay's Casebook you see this characterized in the battles between Dr Finlay and Dr Snoddie)
Slide 9
So to sum up:
The pre war system overall had severe problems-it was a patchwork with uneven access and distribution.
And its finances were under strain- both for the hospitals and for the insurance sector.
There was a rising demand for better planning in the 1930s coming from a variety of sources- the PEP report on the British Health Services, the BMA was working with the TUC, the Socialist Medical Association also was an influential force.
Slide 10
Rapid change came about in war time. We move now to the immediate origins of the NHS.
Firstly the hospitals were reorganized into a more coherent system. The Emergency Medical Service was set up in 1939 and saw the regional organization of hospital provision because of the threat which bombing was thought to pose to the general population. There were other early attempts at regional organization of hospitals via the Nuffield Provincial Hospitals Trust based on experience in the Oxford area.
The Beveridge Report on Social Insurance in 1942 created the idea of a common ' risk pool'
Planning was underway for the service throughout the war as part of the work of the coalition government. A key document prior to the NHS was the 1944 White Paper under the aegis of the Conservative Minister of Health Henry Willink whose picture is on this slide. The service was to be based in local government, but organized through joint authorities which would also run hospital and consultant services. There was to be a hierarchy of professional expertise parallel to the elected voices of local councilors with a Central Medical Board and health centres also part of the plan. It was an attempt to satisfy all parties not least the Conservative and Labour interests in the coalition administration.
But a major plank of opposition was the medical profession itself. The BMA opposed any move to a salaried medical service and local authority control of health services for two reasons:
• the threat this offered to clinical freedom
• the echoes of Nineteenth Century systems of lay control through friendly societies and the Poor Law.
So the 1944 White Paper might have offered a more responsive system but it was unacceptable to the key professional interests.
Then came the Labour victory of 1945, Bevan's appointment as Minister of Health and the NHS Act of May 1946 which changed the previous proposals. Bevan espoused the nationalization of the hospitals (state ownership and control under appointed local bodies) rather than local authority control which had been Labour Party policy until then.
Conflict however, still continued with the medical profession right up to the appointed day 5 July 1948 and as late as April it looked as if the doctors would not join the new service. But there was also division in the profession which Bevan exploited. There was conflict also between the Royal Colleges and consultants led by Lord Moran and the GPs and the BMA, Charles Hill and Guy Dain- and within the GPs between the wealthier and poorer ones who stood to gain from the NHS.
You can see in the cartoon at the bottom of the slide Bevan administering rather unacceptable medicine to the profession.
Slide 11
Let us turn to the NHS and what it comprised at the start:
It was free at the point of need- the famous phrase 'universalizing the best'.
It was funded out of direct taxation, not health insurance or local rates.
Let us look at the structure which is shown in this diagram of the time.
There was nationalisation of the hospitals under regional structures of local authority and voluntary hospital representatives.
GP, dental, optician and pharmacy services came under local Executive committees, half professional and half lay. GPs remained independent contractors and were not salaried. Webster has commented that the NHS GP system was effectively the transference of the old panel system into the NHS.
The sale of practices was abolished.
The service was completely free until 1951 when charges were imposed for prescriptions, teeth and spectacles.
Local authorities had a limited role with responsibility for health centres, clinics and services such as health visiting.
The key changes were the nationalization of the hospitals and the reduction and removal of local authority control.
Its important to remember as the diagram shows it was a tripartite structure and the health centre shown on the diagram, was intended to be the unifying mechanism, bringing the different arms of the service together.
Slide 12
Let's stop and see what the coming of the NHS meant to one family.
"I well remember our Brian being born. He was delivered by a doctor up at Oldham, a Scotsman, he got called up and killed in the war, so we never paid for Brian. The doctors were very good. You'd go to the doctor. He had your name and address. And after, you'd got a bill, and if you couldn't pay it, which very few people could, each doctor had his own collector. The collectors used to come round each week and you'd pay sixpence. My wife's father and mother used to say they'd never be straight in their lifetime. When the National Health came in all those doctors' bills were written off. The collectors used to be the same type who were park keepers in them days-they'd be no use today, kids'd throw them in the pond - but they were always little wizened fellers."
Slide 13
There have been many historical debates about the NHS and its origins. I'm going to mention two of them.
One is the debate about conflict or consensus. Did the NHS come about through consensus - or did it have to be fought for?
The political scientist and historian Rudolf Klein has argued that the NHS came about through consensus- what he means is that gradually most interest groups and movers and shakers in terms of power accepted that there needed to be a national system. He sees this consensus gradually developing through the interwar years and during the war. In his view the NHS as established by Bevanwas merely a step further than previous plans and based on them. Klein has been supported by other analysts such as the US historian and policy analyst Daniel Fox, who has argued that the principle of what he calls 'hierarchic regionalism' was behind the reorganization of many Western health services during these years. These commentators tend to stress the role of central bureaucracy and also of interest groups rather than party politics which they regard as rather like the icing on the cake.
Charles Webster, official historian of the NHS, however takes a different view-he argues that the NHS had to be fought for in the form it eventually took and that the role of civil servants in the MH and of the labour movement was important. This chimes with recent work by an American political scientist Lawrence Jacobs who argues for the increasing importance of public opinion within politics during the war and as also affecting the culture or climate of opinion in which officials were working. Webster argues that ends and means cannot be disassociated .
The other area of debate has been in the assessment of Aneurin Bevan and his achievement. We've already seen how the final settlement was very much his responsibility. Look at this cartoon which shows him administering social responsibility capsules to medical vested interests.
The doctors initially did not look favourably on him because of the connections he had had as a young man with the medical aid society in his home town of Tredegar. They thought he was coming from the hated club practice tradition. He was known to have supported both a salaried service and health centres. But he was pragmatic and dropped both of these. According to one Labour MP his greatest success was with his own party.
'the way he applied the anaesthetic to supporters on his own side, making them believe in things they had opposed all their lives.'
Assessment of his achievement by historians and others has been mixed. If you look at Michael Foot's biography of him, its full of admiration (Foot was Bevan's successor as MP and idolized him) It is adulatory and this is the line which has often been taken by key politicians who use Bevan's achievement in 1948 as totemic in their own present day plans. He appears in a less sympathetic light- as might be expected 'in Philip Williams' biography of Hugh Gaitskell, in particular over the later history of NHS cuts.
And historians recently too have been critical. Both Frank Honigsbaum and Rodney Lowe's recent work on the welfare state have argued that the NHS was an opportunity missed rather than seized.
The issue of the salaried service and the payments made to consultants to induce compliance with the NHS have come in here. Bevan rejected the salaried service saying,
'I do not believe the medical profession is ripe for it. There is all the difference in the world in plucking the fruit when it is ripe and plucking it when it is green.' Maybe a salaried service could have developed alongside health centres if these had been offered to Regional Hospital Boards to run. Bevan might have negotiated harder with the medical profession and secured a settlement with fewer hostages to fortune for the future (for example over private medicine and a salaried service). But its easy to say this at a distance from events.
This brings us to
Slide 14
Successes and problems - let us look at these.
Access for all was very important in particular for women. The new service had great popular support and the removal of the fear of illness and inability to pay cannot be overestimated.
It coincided with advances in medicine and technology and drugs- penicillin, TB vaccination and treatment, drugs for mental health and blood transfusion. It was a sickness rather than a health service. Infant mortality went down rapidly .But these developments were happening in many countries at this time irrespective of the system in operation.
We should also remember it was a period of tremendous change in patterns of disease- the change from infectious and epidemic to chronic disease and the 'diseases of affluence'. It was a period of great optimism about health and the possibilities of technology and the new service.
There were some criticisms of the new service which were challenged at the time and have also been challenged since.
Overspending was one of them. The NHS was said to be financially profligate with a torrent of free teeth and specs. But until 1960, NHS share of national wealth measured through Gross Domestic Product (GDP) actually fell. This low cost was confirmed by a committee established by the Conservative government in the 1950s, which produced the Guillebaud report. After that it did rise from 3.9-5.5% of GDP from 1960- 75.
Recent work by Tony Cutler at Royal Holloway College has pointed to another reason -that the financial projections for the new NHS were in any case flimsy because the planners in the Ministry of Health had been expecting it to be based on local rates rather than central taxation. Although the pre war service had an insurance base, in fact 40% of overall funding in the late 1930s came from the rates and this proportion had been rising pre war.
It was also criticized for being a top down centralized service. Was it a centrally run service? Gorsky's work shows how local figures carried over into the new hospital boards and committees. Some of our recent work on local activities in the alcohol field in Nottingham in the 1960s and 70s shows how much room there was for local manoeuvre.
Other criticisms were well founded.
Services continued to be poorly integrated- it was a three fold system and health centres did not take off for various reasons-cost and doctor opposition among them. The NHS was a doctor dominated service.
And the democratic input from having the service located in local government was lost. Its important not to see the local government service pre war as a golden age of popular participation- but the opportunity for local participation had been there .Some of the accounts which historians have written of the MoHs in the Town Hall show a very different way of operating. Paddy Donaldson, the father of the current Chief Medical officer Sir Liam Donaldson, was one of the last MoHs in the 1960s.His autobiography show how the MoH worked within local political structures and used them.
But some of these issues had a longer history even than 1948.
The problem of the interface between health and social care dated from the days of the Poor Law - and the close relationship between doctors and the state from 1911 NHI. Doctors always looked to government to resolve their problems which they did not do in many other European countries.
Lets now turn finally to how those issues pan out in the present,
Slide 15
Current issues with a history:
1. All health issues are political at the centre- health occupies greater space in our media then elsewhere. We expect the government to be directly responsible. Its back to the Ministry of Health and parliament in that first slide.
2. Integration of services on the ground at the local level is still an issue- the health and social care interface and joint planning is very much a matter of discussion and concern. Local authorities now have their health scrutiny committees and there are some joint health and social care trusts. Some Primary Care Trusts (PCTs ) are coterminous with local authority boundaries. So there are ongoing attempts to solve this historical problem.
3. The boundary between specialist and GP services also continues as a key issue and is currently on the agenda because of the Darzi proposals for London and continuing discussion. Darzi has put forward the idea of 'polyclinics' to attempt integration of specialist and GP services. This is the old health centre idea reborn. It has been presented as new or European (Berlin is given in the report as an example) but of course it is not. I have talked about its earlier incarnation today and it had a wider history .In the interwar years there were health centres run by local authorities, such as Finsbury and Bermondsey among others and also the Peckham Centre which has attracted recent attention for its holistic approach .The Finsbury centre is shown on this 1942 poster about post war planning-it epitomized what was intended for the people's health at that time.
4. What about the democratic deficit? Some are arguing for greater localism now - there is -'new localism-' and a desire for more democratic input. The Labour government is still struggling with how to involve the patient and is on to its latest reorganization of patient input. Liberals have proposed elected health boards.
5. There are also issues of resource allocation in a centrally directed system which have been on the agenda on and off since the 1970s and even since the early discussion in the 1950s. In the early days it was the consultant who decided on rationing and who received treatment .In the 1970s we had the work of RAWP (Resource Allocation Working Party) and of the Black Report. NICE (National Institute for Clinical and Health Excellence) is one of the latest mechanisms to try to resolve this dilemma both in terms of interventions and the availability of treatments and drugs.
6. The role of public health and prevention was always the poor relation and this lost its role in local government totally later on. There have been recent attempts to raise its profile in a broader way in particular through the recent Wanless Report.
7.There are many other echoes from the past which could be mentioned for example, the role of private medicine which had its place in the early NHS and lost it in the 1970s with pay beds .Its reinvolvement now has different locations-as for example in Independent Treatment Centres. The recent decision to involve an American health care company in general practice in Camden has aroused intense opposition in part because it brings with it echoes of the sale of practices which Bevan abolished in 1948.
But there are other echoes too. The foundation hospital trusts, for example, were justified by John Reid as inheritors of the working class mutual tradition. But they seem more akin to the old voluntary hospitals reborn.
The recent decision to devolve some aspects of primary care to local pharmacists also draws on that historical tradition I have mentioned of counter prescribing.
This is my final point- the importance of history. The NHS is not without its historical allusions. Alan Millburn and John Reid as health ministers in particular were fond of looking to the past and invoking the spirit of Bevan, Patrician Hewitt did this more recently. But there are great swathes of NHS and pre NHS history which politicians seem to know little about .And those planning for the NHS now often seem ignorant of history- the Darzi reports are particularly notable for this lack and seem to operate in a history free zone. They should take more account of history in their analysis of policy options for the future-for the NHS in its 60th year cannot escape from its history.
©Professor Virginia Berridge, Gresham College, 14 April 2008
This event was on Mon, 14 Apr 2008
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login