Twenty-first Century Threats: Tuberculosis
Share
- Details
- Transcript
- Audio
- Downloads
- Extra Reading
This lecture is a part of the series Twenty-First Century Threats. Other lectures in this series include the following:
HIV/AIDS
Malaria
Lyme Disease
Download Transcript
26 March 2012
Twenty-first Century Threats:
Tuberculosis
Professor William Ayliffe
I am very grateful to Gresham for giving me the chance to do this. My sabbatical this year was actually taken because I contracted tuberculosis and had to be treated, so I was unable to see patients for a while and needed to get myself well. This disease was thought to have been conquered, but in fact, it has not, as I found out to my cost when working in Africa.
This is a portrait of one of the most beautiful women of her day. She was the muse of the Pre-Raphaelites. In this particular picture, she is dying, and she is being painted by her husband, who was so distraught at her death that he could not move from her coffin for four days.
This is a life mask of John Keats, from when he had tuberculosis. Keats was coming home late in the evening, after a drink in the city, on the outside of the coach back to Hampstead. It was a cold night, and when he got into his house, he coughed a bit and felt a metallic taste in the back of his mouth. He then spat it into a handkerchief and called to his friend who lived with him, “Brown, bring a candle!” He brought one over and they looked into the handkerchief and saw it was bright red, which Keats identified immediately as arterial blood. He said to his friend, “This is my death knell,” and he was absolutely right, as events were to unfold. Things started to move rapidly. They brought in Dr Bree eventually, for a second opinion, after Keats had been bled repetitively by the local surgeon. In fact, after one particularly severe bleed, the surgeon came in to bleed exactly the same amount of blood from his arm.
Bleeding was a very important way of treating diseases in those days, whether the patient was ill or bleeding or not. There is a famous story in the Battle of Waterloo, where the colonel of the Coldstream Guards finds one of his soldiers, who has had his leg blown off, bleeding from the femoral artery, while simultaneously being bled by the military surgeon - from the arm! Unfortunately, as he takes off his belt to use it as a tourniquet, the Coldstream guardsman dies.
Keats qualified as a doctor, but decided to be a poet (he must have been mad and hysterical), diagnosed his condition as being no organic disease. He changed his diet, believing that he needed to eat red meat and red wine every day and go for walks. Under this regime, Keats actually made a rapid recovery and became a lot better, so much so that he felt he could take his suit with Fanny Brawne a little bit further. Unfortunately, it did not last. He suffered some more haemorrhages, he was bled again, and finally, being so ill, he decided to go on a trip to Italy, taking leave of Fanny Browne. They exchange some hair and she gave him a stone that she used to hold to keep her hands cool in the summer, which he took to his grave.
Unfortunately, the journey was awful – they were blown about by winds. They arrived in Naples, where they were quarantined, because of an alleged cholera outbreak in London. Eventually, they made it to Rome, where they took up lodgings and came into the hands of the local doctor, Dr James Clark. He listened to Keats and, with great diagnostic acumen, said, “The lungs appear to be sound”. He prescribed a dainty diet and bled him. The dainty diet consisted of one anchovy a day, and his wife produced a concoction containing antimony, a deadly poison. Keats went through terrible suffering.
There were concerns that his condition was made worse by the terrible reviews his poetry had been receiving. His great collection of poems was described as “imperturbable drivelling idiocy” and they recommend to Keats that “It is a better and wiser thing to be a starved apothecary than a starved poet, so back to the shop, Mr John, back to plasters, pills and ointment boxes.”
This set him back further, and eventually, with terrible suffering, over many days, he died in agony, not being allowed the laudanum that could have given him some relief. In his last letter to Fanny, he says: “I have left no immortal work behind me, nothing to make my friends proud of my memory, but I have lived the principle of beauty in all things, and if I had had time, I would have made myself remembered.” In fact, during the last day of his life, he was tortured further by his friend, an ardent Christian (Keats was an avowed non-believer), who persisted in reading Christian tracts to him.
Byron said of Keats:“Tis strange in the mind that a very fiery particle should let itself be snuffed out by an article”; Shelley, “The loveliest and the last, the bloom whose petals nipped before they blew, died on the promise of the fruit.” Indeed, we lost one of our greatest poets from this dreadful disease.
Kathleen Kelly was born to a slightly impoverished retired East India Army officer. He was retired after the Indian Mutiny and sent back to England, as the British Raj came into effect. He arranged for his daughter, aged seventeen, to be married to one of his acquaintances, a surgeon in the Indian Civil Service: Isaac Newton. Unfortunately for her, on the outward journey, she was seduced by Captain Palliser, possibly of the Bengal Rifles. She confessed to this on her wedding night (never a good thing to do), which greatly upset the Christian doctor. He sent her straight back to England, where she became the mistress of Palliser and eventually had his baby, but did not marry him.
In 1872, she met James Tissot, the most commercially successful painter of the day (although Oscar Wilde did not rate him, referring to his subjects as “common”). She became pregnant by him. She started to cough. Tissot moved this Irish divorcee and two illegitimate children into his house, and you can imagine the consternation this creates amongst the neighbours, particularly in those days. As tuberculosis took hold of her, she became unable to bear Tissot’s grief any longer, and so took an overdose of laudanum in November 1882. Tissot sat by her coffin for four days. Being a Catholic who committed suicide, she was buried in unconsecrated ground in Kensal Green Cemetery.
Millais’ famous and controversial painting Ophelia was, at the time, denigrated in the Times: “something strangely perverse in an imagination which souses Ophelia in a weedy ditch, and robs the drowning struggle of that lovelorn maiden of all pathos and beauty.” Elizabeth Siddal, the model for this painting, was born in Hatton Garden in 1829. She married Rossetti, posed for Millais an hour at a time in a cold bath. He did put some candles under it, but they would often go out, and Millais, being so absorbed with his painting, would forget to relight them.
Unfortunately for Elizabeth Siddal, she became very ill with pneumonia, contracted TB, and was sent off to France by John Ruskin. Struggling to cope with the TB, she also committed suicide by laudanum. This added an edge of irony to Millais’ comment, that “the circumstances under which I had to paint this painting would be a greater punishment to do that than a murderer to go to hanging.” Unfortunately, his muse died.
So, what was this terrible scourge that was killing the young, the beautiful, the intelligent, by their tens and their thousands, and the poor and the working classes by their millions?
It was the result of a tiny rod, one-thousandth of a millimetre. They grow very slowly, leaving classical waxy coats. It is very difficult to grow. It is actually not just one organism but a group of cousins that are very closely related, called the mycobacterium tuberculosis complex. They include mycobacterium bovis, which infects cows and badgers and was one of the reasons pasteurisation was introduced. There is the BCG variant of this, which was developed as an immunisation against tuberculosis in the 19th century. There are a couple of varieties that occur in Africa, and seals and voles have their own types.
Genomic studies show that this is a very stable gene. It looks as if it was present in very early humans, as they migrated out of Africa. Furthermore, the proto-tuberculosis found in these people evolved later into the second lineage, which included mycobacterium bovis and caprae: the probable source of animal tuberculosis. It seems to occur at about the same time as domestication of animals.
This organism is slow to grow, tough. Why? Well, a normal rod has a normal lipid cell wall. Around the bacterium there is a very tough protein sugar coat, in layers, which stains purple with certain dyes. TB is different. Outside, it has a very thick waxy coat. In fact, about 60% of the whole cell wall comprises this waxy coat, which makes it very difficult for antibacterials to get into it to kill it, and very difficult to get stains in to identify it. It is very difficult to kill it if you bleach it or add acid. It is very difficult to kill when it enters the body, because our ‘killing mechanisms’ cannot penetrate the thick, waxy membranes.
Now, TB is with us today. It has not disappeared. It is just not in the places where it used to be. It has moved out.
Dr Livingstone wrote a letter stating that TB did not exist in Africans who had not come into contact with Westerners – it did not exist in Samoa, for example. In one instance, a ship from Bristol went over and one of its crewmen began coughing blood. He begged to stay and the captain said, generously, “You can stay on this island if you like – furthermore, I’ll let you stay with a friend, and we’ll come back and pick you up next year”. Amazingly, the ship returns the following year, to find only two people alive on the island – the crewmember and his friend. All the locals had died from tuberculosis.
In native populations, this disease could spread very quickly, and was probably one of the causes of death of many American-Indian tribes. Even as late as 1930, Native American tribes were suffering greatly, with a much higher mortality than the people who came from Europe. The situation was similar in Australia, with its aboriginal population.
TB is much more frequent in Africa, the Far East, parts of Russia and parts of Latin America, as we shall see later. The incidence of TB in England started to fall about two or three years ago, but we do not know if that is just a blip in the statistics and the figures will start to rise again. Certainly, there has been a dramatic increase over the last two decades, and over different areas. I work in Croydon, which has quite a high incidence of TB, whereas Hampstead probably does not. The same was true even in the 1800s.
The United Kingdom has a slightly higher level of tuberculosis than Austria, France, Greece and Germany. If we put this in a global perspective, we see that incidence in Angola, Nigeria and Jamaica is low; Zimbabwe, however, has one of the highest incidences in the world, at over 600 per 100,000 - an astonishingly high rate of tuberculosis.
The organism enters the body in various ways, most commonly through the lungs. It is picked up by the local innate immune system, with toll-like receptors and gamma-delta cells, and is shipped off to the local lymph nodes. There, it starts to stimulate the immune system, which forms a granuloma. Remember, this bug may not be killed. It is very waxy, hard to kill. It can survive in here for years or even decades, still alive – not growing, but not killed either. Sometimes, the by-products of this slow process form a cheese-like material called caseation. This contains the remnants of the waxy cell walls, the cold pus and remnants of the white cells, and also, on occasion, one or two live TB vasili.
Pulmonary disease is the most important TB-related condition, formed by a little tiny focus on the outside of the lung, usually in the top sections. Extra-pulmonary tuberculosis happens when it gets outside the lungs, when the granulomas burst into the bloodstream and spread all over the body, forming little milliary dots.
In 3% of cases, this type of TB is lethal before antibiotics, and rapidly lethal, as we can see from the story of Thomas Wolfe, the great North Carolinian writer. He fell ill while travelling in Seattle and, comatose, was shipped over to Walter Dandy at Baltimore. Dandy attempted a life-saving operation, but the disease had totally rotted the right side of Wolfe’s brain. Without regaining consciousness, he died. Milliary TB was greatly to be feared.
TB can even affect the eyes, sometimes from a distant focus elsewhere. Having a massive inflammatory response, it can blind you. Or, it can occur from disseminated TB, milliary TB, causing tiny dots to appear throughout the choroid in the back of the eye. The choriod has the highest blood flow of any tissue in the body in order to cool the retina down.
TB can also affect lymph nodes, forming scrofula. The name scrofula means ‘little pigs’, as that was what the ancients thought it resembled. In adults, this is caused by mycobacterium itself; in children, it might be formed by a sub-strain. It is a cold abscess, and the local skin acquires a very deep purple colour.
Did TB exist before human beings? It just might have done. Some evidence comes from a stone quarry in Turkey, where bones were found showing inflamed vessels – possibly inflammation from tuberculosis. There was a lot of fuss made about this discovery.
Why might they have got tuberculosis? Homo Erectus, the first Homo species to leave Africa, was dark-skinned. As a result, he did not take in the sunlight, and therefore, did not take in the vitamin D formation necessary to fight this disease. Consequently, he may have been particularly susceptible.
We are on firmer ground when we come to ancient times. We know that TB affected the skeleton, with a predilection for weight-bearing joints, particularly the spine, called Pott’s disease or Pott’s fracture. This affected about 3-5% of people, even in the 1950s. We have pictures of Pott’s fracture on the wall of Ipy’s tomb. We have Mrs Cecil Firth’s 1910 drawing of Pott’s disease in a mummy, which shows the deformity clearly. There are also references in the Ebers Papyrus to consumption associated with neck lymph nodes and some recommendations on treatment.
We are even firmer ground when we look at the pathological tissue itself. Dr Granville’s mummy was originally dissected in 1825, with a full report submitted to the Royal Society. As the dissection was carried by a gynaecologist, they thought that the mummy had died of a gynaecological tumour of the ovary. This was subsequently discovered to be a benign adenoma. However, histology of the lung demonstrated a fatally pulmonary exudate, and an analysis of this and other tissues has shown that there are mycobacterium cell products present, particularly the mycolic acids, those resistant waxes that last for decades or thousands of years if they are preserved in the right way. So, even when we cannot extract DNA from tissues, we are able to use many other modern techniques to see if tuberculosis was present. Interestingly, in the case of the mummy, they did manage to extract some DNA. A lot of fossilised and mummified DNA is often fragmented and it can be very difficult to get positive results from it, but in this case, they succeeded.
We are on firmer ground still when it comes to TB in the Iron Age. Skeletons from this period have been found in Dorset and Southern Siberia with Pott’s fractures. In Siberia, they found mycobacterium bovis DNA. Clearly, close relationships between people and their animals, as well as between people and their families, can lead to tuberculosis. A similar thing happened 2,000 years later in Manchester, which I shall come to shortly.
There are several potential records of tuberculosis to be found in Ancient Indian, Chinese and Greek literature, but the first really recognisable and systematic description of a patient with TB comes from Aretaeus.
Not a lot happens for a long time. Paracelsus suggests that TB is “a failure of an organ in its alchemical duties, and in the lungs, stony precipitates develop”. Francoise de Bouve found tubercles in the lungs, which he identifies as the origins of the ‘phthisis’ (i.e. the wasting). He writes that “phthisis is the scrofula of the lung”.
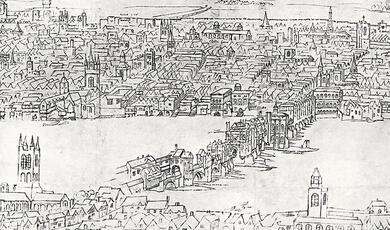
In the seventeenth century, pulmonary TB became rife in London. Locke estimated that 20% of all deaths in London at this time were from phthisis. Christopher Bennet wrote a book containing a handy couple of diagrams on how to make inhalers. People loved this book. It was full of really interesting and useful tips and case reports. Thomas Willis wrote a chapter on phthisis, arguing that consumption arises from “a fault in the lungs”.
Richard Morton (1637 – 1698) was probably one of the most boring writers in the whole of the English language. He trained as a vicar. He was unable to comply with the Act of Uniformity and was therefore kicked out of England. He disappeared. We think he might have gone to Leyden, where he reappeared under the patronage of the Prince of Orange, a Fellow of the Royal College of Physicians, in 1678, and wrote a book. This book is important because he was using the old Dutch teachings of 50 years before, stating that the “consumptive cough proceeds from a glandular swelling or a tubercle of the lungs themselves”. Unfortunately, his work is steeped in Galen, and he interprets this as a glandular degeneration. However, he points out that, since so many people were dying in the City of London, “the preventing of consumption is the great business.” He believed that TB was caused by an imbalance of humours and a number of predisposing causes, such as: “Troublesome passions of the mind”, “night studies and long watchings”, “foggy and thick black air” and “hereditary disposition”. This latter factor would be considered the most important cause of consumption for the next two and a half centuries. Even today, we still believe that there may be hereditary factors involved in susceptibility to this disease.
Richard Blackmore (1654 – 1729), another very turgid read! Alexander Pope actually calls him “the avatar of dullness”, someone sent down from the gods in a human form to be dull. “The disease we in English call consumption is, in the Latin tongue, called Tabes, and, in the Greek, Pthisis... The essential and distinguished character of this was the wasting of the body.” He thinks it is due to “an ulcerated state of the lungs, with a cough, a discharge of purulent matter, and a hectic fever”. You would not believe the night sweats that I suffered with TB. The weight loss is also very rapid: two and a half stones in just over three weeks. You become emaciated very quickly and extremely tired.
Then we come to the Industrial Revolution. Long Millgate in Manchester was described by Friedrich Engels in The Condition of the Working Class in England as “Hell on Earth”. You passed through alleyways so narrow that two people could not pass together into the septic dwellings behind, ankle-deep in filth and human waste. One room would house a family, a median of five people – and those were the lucky ones. Excavations in Manchester are revealing the basements where the unlucky ones used to live, often five families to a room. There is a solicitors’ office in Manchester where, if you ask nicely, they will show you one of these dwellings, beneath the floorboards. It is about half the size of this room, in which eight families hot-bedded, in between their shifts. As one family came up through the floorboards to go off to work, the next family were coming in to go to bed. Linen was never changed. They stayed down there with their consumptive coughs, passing on the disease to their children.
Alexis de Tocqueville said: “From this foul drain, the greatest stream of human industry flows out to fertilise the world. From this filthy sewer, pure gold flows. Here, humanity attains its most complete development and its most brutish. Here, civilisation works its miracles, and here, civilised man is turned back almost into a savage.”
Between 1790 and 1840, under these conditions, TB explodes – first in this country, then Germany a few decades later, then France, then Italy and finally, near the turn of the century until 1910, Norway. In fact, in the 1880s, it was thought that tuberculosis did not exist in the far north of Europe. But it followed the rest of Europe.
In 1769, children were collected from London workhouses and shipped to Manchester, where they would be put to work until they died. There was no attitude of responsibility or care because there were many more children to replace them. Their life expectancy was very short.
So, in 1833, the Factory Act was brought in by Lord Althorp, limiting the hours that children could work to ten hours a day. This was considered to be a great advance, but it was controversial and split the parties. Melbourne, a Liberal, and something of a mentor to Queen Victoria, voted against it, and Palmerston voted for it.
In 1829, one in four births were stillbirths - an astonishingly high figure. Half of these were born to consumptive or scrofulous mothers. In London, the poor parishes had four times the mortality of the rich. In Dublin, 36% of dwellings consisted of one room, each housing an average of five people.
Overcrowding occurred in prisons but also, surprisingly, in nunneries. When you were admitted to a nunnery, you were given a health examination to prove that you were clear. You then went into the nunnery and, on their strict diet, you had an average life expectancy of three years. Many of these young girls hallucinated, leading to pilgrimages that are still followed today.
Marie Duplessis, one of the most beautiful women of her age, married a very rich Englishman who died of tuberculosis. Subsequently, she became the lover of the young Dumas. He then wrote the story of Armand, who falls in love with a courtesan, a love forbidden by his father. In atonement for her sins, she tries to make Armand believe that she does not love him anymore. This became the plot of Verdi’s La traviata.
Napoleon II had an appalling consumptive death. He had grown up avoiding tuberculosis; his father spent tens of thousands ensuring that he came from clean stock, that his mother did not have tuberculosis and was a virgin, that the family did not have tuberculosis, and that he grew up in open and airy rooms (a whole suite was built for the young child). Nevertheless, it did not stop him getting tuberculosis, and he died a horrible death, with taberculis laryngitis and foul diarrhoea. His mother had been estranged since the great Napoleon had left the scene, and arrived only when he was unconscious and she was unable to say goodbye to him. However, she had ignored him for most of his life, so I do not think there was too much love lost there.
Following his death, there was a mad rush to collect locks of his hair, and the body was left completely scalped. This was not usually possible in Europe. Normally, you burnt the bedding because it was thought to be contagious.
In Edmond Rostand’s play, L’Aiglon, in which Sarah Bernhardt plays the young Napoleon, he does not die this horrible death. He dies making an escape from his prison, from the Hapsburgs, trying to become the king once more. On his way to Poland, he crosses the field of Wagram, where his father had caused so many deaths in that appalling battle, and he hears the cries of the dead bodies. His friend Taliband is then shot dead by the pursuing Austrian troops and Napoleon feels that this is some form of atonement for the sins of his father.
This idea of somehow ‘deserving’ disease and illness - “What have I done wrong, doctor?” – existed then and still persists today. We have not escaped from these medieval concepts of illness. We still believe that mental illness is the fault of the person suffering from it; we still think that alcoholism is a slightly wayward and eccentric behaviour, rather than a disease. I just want to emphasise how little our attitudes in this regard have changed.
Historically speaking, percussion has always been the first step towards diagnosing tuberculosis. It was invented by Leopold von Auenbrugg, the son of an innkeeper, who was used to ‘percussing’ barrels to see how full they were.
Jean-Nicolas Corvisart made an advance in this field by using something called a pleximeter.
When an English doctor later forgot his pleximeter, he used his middle finger, which is how we now percuss. You can percuss yourselves tonight, in the bath. People became so good at this that they were able to diagnose the tiniest of nodules.
William Osler’s favourite possession was a referral letter from a doctor in Harley Street who had percussed his lung. “He has a tuberculous lesion the size of a walnut shell in the left upper lobe” – something that the doctor had discovered, in the days before x-rays, by just percussing and listening.
These doctors were tremendously skilled people. The problem with listening to the chest was that the process could be a bit disgusting. You could lay a silk handkerchief on it, if you were rich, but if the patient was fat you had to lift up an enormous pendulous appendage in order to apply your ear. As a result, Laennec invented the world’s first stethoscope, with which he was able to diagnose all sorts of things happening in the lungs. In fact, it is claimed that his nephew, Meriadec, diagnosed tuberculosis in Laennec himself, using his own instrument.
This piece of equipment was controversial, and even as late as the 1950s, the founder of the American Heart Association refused to use a stethoscope and walked the wards with a red silk handkerchief.
Of course, the invention of x-rays made things a lot easier.
Now, what was the cause of this strange disease? We can now diagnose it. We know what it does, we know it kills you, we know it is associated with poverty, we know it is associated with all manner of foul and unholy things. But what was it?
Girolamo Fracastoro (1478 – 1553) suggested that it might be something called a fomite, which comes from things like clothes. This was not a concept of a living organism, although, interestingly, he is the guy from whom we derive the word “syphilis”. He mentions it in his poem about a shepherd boy, by the name of Syphilus, who angers the sun god of Haiti.
Benjamin Marten, however, took things a step further and proposed that it was a living thing, an animacula – similar to the organisms seen by Anton van Leeuwenhoek under the microscope, 80 years earlier.
Jean-Antoine Villemin (1827 – 1892) was the first to show that this is an infectious disease. He was orphaned at the age of thirteen and went to live with his uncle, a retired soldier. Eventually, he was conscripted in the 14th line and enrolled as a surgeon. He went to the military medical school, where he qualified as an army doctor and was transferred to the Val-de-Grâce military hospital in Paris. He carried out a study in which he took pus out of humans and cattle and transferred it into rabbits. The rabbits got the disease – a fantastic discovery – but he was completely ignored by the scientific community.
Then, along came Heinrich Koch (1843 – 1910), who was credited with discovering this. He identified TB through infecting guinea pigs with material from patients and cattle. He demonstrated that the disease was the same in all cases, shown under slides which had been specially stained. The audience listened to his findings in shocked silence. He was awarded the Nobel Prize in 1905.
Paul Ehrlich was at that lecture, and upon receiving his own Nobel Prize in 1908, he said: “I hold that evening to be the most important experience of my scientific life.”
Koch was lauded, taken to Paris, given the Medal d’Honor and a large dinner. This infuriated Villemin, who said, “We French did this first!” His protestations were eventually dismissed as “the ravings of the maddened vet” (his licence allowed him to practice on both horses and soldiers). He was not considered to be a real doctor, like those who had been to proper universities.
The act of staining is fascinating in itself because, as I have told you, it is difficult to stain waxy things. Hans Christian Gram (1850 – 1938) invented the stain, but TB did not stain consistently. Paul Ehrlich decolourised the whole thing with nitric acid, revealing the bacterium.
Now, not everybody accepted that these bacilli caused tuberculosis (or in fact any disease). Professor Max Pettenkofer was sent a vial of cholera organisms by Koch to try and persuade him that this was a disease with bacteria. During a lecture, he downed the flask in one go. There were gasps of amazement and people fainted. It should have killed him, but it did not.
Bovine TB is quite important, mainly for historical reasons. A ‘wasting’ of cattle has been known for a long time, particularly in Germany, but 40% of cattle in England were also infected in the 1940s. It is normally transferred from cows to humans, not the other way round, and also not from humans to humans - but it can happen. In 2007, six people clubbing in Birmingham passed TB onto each other, but only one of them had any exposure to animals and unpasteurised milk (the presumed source of this). One of these people died, despite the best of treatments, from meningitis.
Now, heating milk had been done a long time before Pasteur. It was carried out in England in the 1700s to prevent rancification of butter and to allow milk to be transported from the provinces into the major industrial towns without it going off. However, even though this was reported in America, it never caught on and is still a controversial topic today. The FDA says you have to drink milk that has been pasteurised. Some of the local farmer dispute this and claim that non-pasteurised milk is good for you – that it can stop asthma. In fact, non-pasteurised milk is the single largest source of injury from any food source in the United States. So, in general, it is considered a good thing to not drink the stuff. However, it is delicious and as a young boy I used to drink it all the time with no problems – and then ended up getting TB later in life from a completely different cause!
We now know that killing badgers is not a good idea because it increases the incidence of TB - not in the area where you kill them, but on its periphery. Sick badgers do secrete TB, but we have to remember that 80% of badgers test negative, and only a small percentage of those testing positive actually excrete TB. So, why are we still killing badgers?
As I have already said, if you pasteurise milk, you are not going to pass TB from cows to human beings, and it does not spread from human being to human being. So, are we doing it to protect the cows? Is bovine tuberculosis such a dreadful thing in cows? Yes, it can be, and also a big economic problem, but you can control this, as we have done. Bovine tuberculosis had disappeared in most parts of England until Foot and Mouth, and then we dropped all the controls, we corralled all the animals together, we replenished stocks with cows transported from areas that had TB, and suddenly we get TB again - no great surprise there!
I have already mentioned an epidemic in the 1800s. ‘Patients of all classes below the wealthy; went to Brompton Hospital and were given a survival time of four years. Go up the road to Harley Street, and 1,000 patients in private practice were given a life expectancy of eight to ten years. So, not only does it infect you more easily if you are working class, it also kills you.
When I was given a tuberculin test, my arm ulcerated because I had also been immunised in the West Indies as a child with BCG. This was meant to save my life and stop me getting TB. The Birmingham girl who died of meningitis had also been immunised with BCG. So, it is not like other immunisations that guarantee a protection. It has a relative protection. It is useful in certain circumstances.
When Koch announced a cure, he was given the Grand Cross of the Red Eagle. However, in 1891 Virchow came along and demonstrated that 21 innoculated patients all died of milliary TB. There was uproar! Koch’s popularity was undermined. He went off to Africa and to Bombay, where he carried out some great work proving that plague is spread by rats. He returned in triumph, was awarded a Nobel Prize, and died after an angina attack following a strenuous cycle of lectures in Berlin.
Meanwhile, a better agent for preventing TB was being developed by the French, at the Institute Pasteur by Calmette and Guerin. This is the one that is used today. The idea came from Norway. If you passage the bug several times on mediums (by several times I mean 230 times, a massive job that takes years) you end up with a bug that is relatively benign in humans.
Phototherapy was introduced by Niels Ryberg Finsen (1860 – 1904), for which he was later awarded a prize. If you go to the London Hospital you will see the statue of Queen Alexandra, consort to Edward VII, who gave the hospital a light for curing tuberculosis. Light is the thing. We suddenly realised that people who overdressed in climates like ours are predisposing themselves to get TB because the sunlight cannot reach the skin and produce Vitamin D.
Collapsing the lung was another method introduced. If you collapse the lung, the bug is starved of oxygen. It cannot spread anywhere. There were many wonderful ways of collapsing the lungs, known as pneumothorax.
It was not all plain sailing, however, as Eric Blair (better known as George Orwell) found out in 1947. He had been treated with a collapse of the lung, but was still dying. They were able to import for him a very expensive drug. By expensive, I mean tens of thousands of pounds worth, more than he had ever earned in his life as a writer. However, Blair gets hypersensitivity and cannot take it, but kindly donates the precious drug to two women in the ward. They were saved and could leave hospital and live a healthy life.
Hugh Feldman, who carried out the original trial on streptomyces, eventually got TB himself. He was treated with a drug but acquired resistance. He was going to die but, luckily for him, Jorgen Lehmann had invented another drug, derivative of aspirin, and which stopped TB using oxygen, thereby killing it. Again, this treatment was very expensive.
Isoniazid, on the other hand, is very cheap because it is made out of coal-tar. Those three drugs formed the cornerstone of modern treatment of tuberculosis, until recently, when multi-drug resistance starts to come in.
We now use four drugs. Some of them are quite toxic, so we do not use them for the whole period. We use them for the first couple of months, wait until we get a clinical response, and then continue with the Isoniazid.
Thank you.
© William Ayliffe 2012
This event was on Mon, 26 Mar 2012
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login