The Evolution of Cancer Therapy
Share
- Details
- Transcript
- Audio
- Downloads
- Extra Reading
Professor Eleanor Stride will discuss the history and development of cancer therapy from its origins in Ancient Egypt - when surgery was the only option to remove a tumour, to the more recent developments of radiotherapy and chemotherapy. She will end by looking at present-day clinical trials that aim to harness the body’s own immune system to eliminate disease (immunotherapy).
Download Transcript
The Evolution of Cancer Therapy
Professor Eleanor Stride
16th February 2022
Introduction
The Price of Longevity
In 2015 a BBC news headline announced that 1 in 2 people in the UK will be diagnosed with cancer in their lifetime, according to a report from Cancer Research UK [1]. In 2017, the worldwide statistics for deaths due to cancer made for similarly depressing reading [2], with death rates apparently increasing by more than 15% since 1990.
Set against this rather dismal picture, however, is that fact that this increase in cancer deaths is largely due to the tremendous success of modern healthcare. Since the middle of the 19th Century, the average global life expectancy has more than doubled [3]. When this is taken into account, the corrected cancer death rate has in fact been steadily falling over the past 2 decades. It is simply that the older we get, unfortunately the more likely it is that we will develop some sort of cancer.
Moreover, for many types of cancer, a diagnosis is mercifully no longer a death sentence. This transformation is due to the remarkable advances in both our understanding of the disease and the corresponding evolution of cancer therapy over the last century. The aim of this lecture is to chart that evolution.
Why Haven’t We Cured Cancer Yet?
Before we look at how cancer therapy has changed, it is important to answer two fundamental questions: What is cancer? and why is it so difficult to treat? In its broadest definition, cancer is the unrestricted growth of malignant cells such that they eventually disrupt the normal function of the tissue in which they are located. In healthy tissue, cells divide in a very organised and controlled manner. If a cell is damaged in some way, e.g., its DNA is corrupted, then a process known as apoptosis – a sort of pre-programmed cell death - is triggered. The cell self-destructs and specialised immune cells (macrophages) are activated to come and remove the debris. This prevents the corrupted DNA from being transmitted to the next generation of cells.
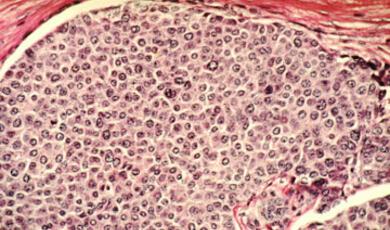
In cancer, however, those finely controlled processes fail to operate. Cancer cells divide rapidly and without restraint, forming a mass or tumour.[1] They secrete chemicals to stimulate the formation of blood vessels to increase the supply of oxygen and nutrients to the tumour. They also manage to “trick” the immune system into ignoring their existence, by displaying certain molecules on their outer surfaces or leaking them into the surrounding tissue. Not only does this allow the tumour to grow unchecked, it also inhibits the normal signals of disease such as pain or fever. Consequently, tumours may become very large and difficult to treat before a patient experiences any outward symptoms.
Unlike normal cells, which simply stop reproducing after 50-70 divisions, cancer cells continue to replicate indefinitely. Consequently, tumours will keep growing until eventually they choke the surrounding healthy tissue. Even before that happens, tumours can become so embedded within an organ, e.g. wrapped around a major blood vessel, that they are impossible to fully remove surgically. In addition, because tumours grow in such an unregulated manner, the arrangement of blood vessels within them is typically highly irregular. This makes it very difficult to uniformly treat a tumour with a drug injected into the blood stream. It also means that some parts of the tumour receive plenty of oxygen and nutrients, whilst others become starved of oxygen or hypoxic. Cells in hypoxic regions change their metabolism and become resistant to most forms of treatment including many drugs and radiation.
Most seriously, cancer cells can develop the ability to break away from the original tumour and spread or metastasise to other parts of the body. Once this has happened, treatment becomes even more challenging. It is normally impossible to remove all of the secondary tumours surgically as there will numerous sites, typically in the liver, lungs, brain or bone. It similarly very dangerous to expose large regions of the body to radiation or to high concentrations of toxic drugs; but a single surviving cancer cell can cause recurrence. Worse still, cancer cells that survive, evolve rapidly to become resistant to whatever they have been exposed to, making the new tumour(s) even harder to treat. Figure 2 summarises these “hallmarks” of cancer that were originally defined by Hanahan and Weinberg [4,5].
There are two further important points to make. First, for the purposes of this lecture, the term “tumour” will be used to refer to a generic solid malignant tumour. There can, however, be huge variability between different types of tumours, between tumours of the same type in different patients, and even between parts of the same tumour. This variability poses a further challenge for developing effective treatments, since what works well in one type of cancer, or one patient may fail completely in another.
Second, we still do not know exactly what causes a cell to become cancerous: inherited genetic abnormalities? Environmental stresses? Failure of the immune system? All of the above in combination? Numerous hypotheses have been proposed, but the origin of cancer remains a topic of intense debate [6]. Fortunately, however, this uncertainty has not prevented its treatment.
From the Ancient World to the Industrial Revolution
Archaeological Evidence of Cancer
Although it is only in the last 100 years or so that we have seen dramatic changes in our ability to treat cancer, it is by no means a modern disease. Pathological analysis of mummified humans from Ancient Egypt and South America has revealed evidence of breast, prostate and bone cancer [7,8].
Recent re-analysis of a human toe bone excavated from a cave in South Africa and estimated to be 1.6-1.8 million years old, indicates the presence of a malignant primary tumour or osteosarcoma (Figure 3) [9]. Evidence of cancer has even been identified in the fossilised bones of dinosaurs from 75-77 million years ago [10].
Moreover, whilst malnutrition and/or infectious diseases were undoubtedly the more common causes of death up to the middle of the 20th Century, cancer may not have been as rare as was previously thought. A 2021 study from the University of Cambridge, analysed mediaeval skeletons from the 6th -16th centuries AD and identified evidence of metastatic cancer in 3.5% of the specimens, suggesting that 9% - 14% of adults were suffering from cancer at the time of death [11]. This is significantly higher than previous estimates of < 1%, although still substantially lower than the 40-50% of adults in modern Britain.
Cancer in Ancient Egypt
Nor was there a lack of prescribed treatments for cancer in the ancient world. The first written examples appear in ancient Egyptian papyri, the so-called Smith and Ebers papyri after the collectors who purchased them in the late 19th Century [12,13]. The papyri themselves date from c.1600 BC, although both are thought to be copies of much earlier documents from ~2500-3000 B.C. The Smith papyrus is famous as one of the earliest examples of the application of the Scientific Method, urging readers to follow a process of “observation, examination and reasoning …” and offering practical advice for the diagnosis and treatment of multiple conditions. These include the use of a “fire drill” (thought to refer to the use of a heated spike to cauterise wounds) following surgical removal of a tumour and numerous recipes containing herbs and minerals including the first documented use of salicylic acid (aspirin).
It is unclear which of the “tumors” referred to in the papyrus are malignant or benign, but the description of Case 45 points strongly towards metastatic breast cancer: “If thou examinest a man having bulging tumors on his breast … that have spread over the breast … [and] thou findest them very cool” the recommendation for treatment is both brief and bleak: “There is nothing.”
The Hippocratic View
The term “cancer” itself is credited to the celebrated Greek physician Hippocrates (460-370 BC), allegedly because of the resemblance of certain tumours to a crab (karkinos). Hippocrates’ teachings, propagated by his successors such as Celsus (c.25BC-50AD) and Galen (c.130-200 AD), dominated medical practice for some 1500 years following his death, and much of his advice remains relevant today. Indeed, whilst his explanation of the cause of cancer – an imbalance in the bodily “humours” specifically an excess of black bile – does not withstand modern scrutiny, his advice for the treatment was highly practical and echoed that of the ancient Egyptians: “That which medicine does not heal, the knife frequently heals; and what the knife does not heal, cautery often heals; but when all these fail, the disease is incurable.” [14] Moreover, though his followers in later centuries would frequently advocate draining of the humours through purging and blood-letting, Hippocrates, himself advised against any form of intervention for advanced tumours: “Occult cancers should not be molested. Attempting to treat them, they quickly become fatal. When unmolested, they remain in a dormant state for a length of time" [14]. Given the tremendous risks associated with surgery at the time, this advice likely saved many patients from premature and painful deaths (Figure 4).
In the absence of a reliable cure, however, most cancer sufferers throughout Roman and Mediaeval times were left to rely on prayer or magical spells, alcohol and opiates to relieve their pain, and a bizarre array of remedies ranging from “Egyptian paste” – an arsenic-based salve quite possibly based on one of the ancient recipes [2] as reported in the Smith and Ebers papyri and passed down through generations of physician-priests - to the truly Macbethian fox lung, tortoise liver and crabs’ eyes.
The Dawn of Modern Surgery
The notion that disease, and cancer in particular, was the result of a humoral imbalance remained largely unchallenged until the 16th Century when advances in anatomy called into question the existence of black bile. Even so, it wasn’t until the mid-18th Century that the Hippocratic/Galenic view began to wane. From a patient’s perspective is arguable whether this was initially beneficial, as it encouraged previously cautious surgeons to attempt extremely risky procedures.
An 1836 edition of a Dictionary of Practical Surgery contained a dramatic reversal of Hippocrates’ advice: “In treating of cancer, we shall remark that little or no confidence should be placed either in internal remedies and that there is nothing except the total separation of the part affected [15].” With modern methods of anaesthesia and asepsis several decades away, many of those patients who survived the pain and shock of the procedure itself died soon after from infection.
Fortunately, by the end of the 19th Century, the pioneering work of scientists and clinicians including Louis Pasteur, Lawson Tait and Joseph Lister had transformed surgery from a life-threatening gamble to a relatively safe and effective operation with the introduction of rigorous sterilisation [3] procedures. One of Lister’s early “antiseptic” operations was the successful treatment of his sister for breast cancer in 1869. Simultaneously, there were rapid improvements in anaesthesia, including the famous demonstration of ether as a general anaesthetic by William Morton in 1846. These radical changes in surgical technique were embraced, amplified and mechanised by the formidable William Halstead, surgeon and Professor at Johns Hopkins Hospital. His advocacy for aggressive surgery as the only way to defeat cancer, had a profound influence on subsequent generations of surgeons and oncologists. His single-minded approach, particularly in the case of radical mastectomy, is no longer favoured; but surgery remains the first line treatment for many types of cancers and is frequently curative.
The Modern Era and The War against Cancer
Radiotherapy
Advances in surgery ran in parallel to a series of other discoveries that would have a transformational effect on cancer treatment in the 20th Century. The first was the discovery by Wilhelm Röntgen in 1895 of the mysterious “X-rays” - invisible beams of energy produced by vacuum tubes that could pass through human flesh (Figure 5). That there might be a potential application of this strange new form of energy in cancer treatment was proposed astonishingly quickly and long before either the true nature of X-rays or the effects of radiation on the body were understood. It is unclear who performed the very first radiotherapy [16], but a widely accepted story is that Emil Grubbe, a medical student in Chicago who had chanced to also work in a factory producing vacuum tubes, noticed that his hands and that of his fellow workers suffered from peeling skin and damaged nails. He hypothesized (correctly) that this was due to the fact that skin cells reproduce at a relatively high rate and so exhibit damage faster than other cells. He further reasoned that rapidly proliferating cancer cells should also therefore be sensitive to x-rays. In 1896, just a year after Röntgen’s discovery, Grubbe treated a breast cancer patient with X-rays, exposing the tumour daily for 2 and half weeks. The treatment was ultimately unsuccessful, the cancer had sadly already metastasised, but the treated tumour itself shrank. In the same year, Victor Despeignes in Lyon and Dr Voigt in Hamburg also treated cancer patients with X-rays, and over the subsequent decade years there was an explosion of clinics offering “radiotherapy” (Figure 5). Boosted by the discovery of radium by Marie and Pierre Curie in 1902, which enabled higher doses and even radioactive implants to be applied, radiotherapy became the leading weapon in the fight against cancer. As early as 1901 it was heralded as “An absolute cure for all forms of cancer [15].”
This zealous enthusiasm was inevitably tempered by clinical reality. Though highly effective against some types of tumour, radiation, like surgery, was of only limited use in metastatic cancer, providing primarily palliative rather than curative effects. The side effects of treatment could be extreme and worse still, prolonged exposure could actually cause cancer. A further issue was also to emerge - radiation-resistance - cancer cells that survive initial treatment become increasingly resistant to subsequent exposure. Consequently, the risk to benefit ratio diminishes significantly with repeated treatment. Thus, although radiotherapy has rightly remained a mainstay of modern cancer therapy, its limitations were clear from very early in its application. It was most certainly not an “absolute cure.”
Chemotherapy
Whilst radiotherapy was being celebrated as a triumph of scientific discovery, alternative approaches were also being explored. In Germany, Paul Ehrlich, working on dyes to improve the staining of biological samples, postulated that if a similar specificity could be achieved with a drug, then a Zauberkugel or “magic bullet” could be produced to rid the body of disease without harming healthy cells. Ehrlich made significant contributions to medicine, including a cure for syphilis and important work on immunology [4], but sadly succumbed to tuberculosis before his concept of chemotherapia specifica could be applied to cancer directly.
An early candidate for a magic bullet for cancer came from an unlikely source. In the aftermath of the First World War, doctors treating survivors of the horrific effects of mustard gas made a surprising observation: that the chemical seemed to target cells located in the patients’ bone marrow. The implications of this observation for cancer, however, were not appreciated until a similar examination of victims of mustard gas during the Second World War. Dr. Stewart Francis Alexander reported that the gas seemed to disproportionally affect rapidly proliferating cells and proposed that it might also therefore provide a means of restricting tumour growth. Pharmacologists, Louis S. Goodman and Alfred Gilman, took this theory and applied it to the treatment of lymphoma. Following successful trials in mice, they moved to a clinical trial and saw similarly dramatic effects on tumour growth. The impact on patient survival in these initial trials was less impressive, but the results demonstrated the principle that a drug could tackle cancer.
In parallel at Harvard Medical School, Sidney Farber was determined to find a cure for childhood leukaemia. The discovery of folic acid in 1937 provided a vital step. When administered to leukaemia patients, folic acid appeared to cause an alarming proliferation of malignant cells. Collaborating with chemists Harriett Kiltie and Yellapragada Subba Rao, Farber developed “antifolates” to block cancer cells from using folic acid. The success of the drug was modest. Initial remissions were impressive but sadly short lived, although the drug (now known as methotrexate) was later found to be highly effective in other cancers.
If methotrexate was not the dreamed of cure, Farber’s success in raising the profile of cancer and funds for research into treatments was unquestionable. He recruited both sporting and Hollywood stars to his campaigns and most notably the redoubtable socialite and lobbyist, Mary Lasker. Their combined efforts and relentless lobbying of the US Senate led to the establishment in 1955 of the Cancer Chemotherapy National Service Centre – an institute dedicated to drug discovery. Coupled with growing commercial interest from the pharmaceutical industry, a battery of chemical agents developed. Mustine (the derivative of mustard gas) was joined by other so-called alkylating agents which work by chemically inactivating DNA to prevent cell division and other antimetabolites which, like methotrexate prevent DNA synthesis by interfering with use of a key nutrient, again to prevent cell division. Other classes of drug would soon follow, including plant derivatives such as Vincristine, Camptothecin and Paclitaxel; drugs borrowed from other areas of medicine such as antibiotics and antimalarials; and platinum- based drugs.
A further key discovery in the mid-1960s was that the combined effect of different chemotherapy drugs could be significantly greater than that of the individual agents and also limited the rate at which cancer cells became drug resistant. Combination chemotherapy is the standard of care today, although like radiation, chemotherapy is very rarely curative in metastatic cancer and its side-effects can be horrendous.
Other Advances
Although surgery, radiotherapy and chemotherapy have become the current “pillars” of cancer therapy: They are by no means the only successful treatments developed over the course the 20th Century. Non-ionising radiation generated by lasers, microwave antennae and high intensity focused ultrasound has been used very successfully to treat localised tumours. Instead of damaging DNA in the way X-rays do, absorption of energy from these sources essentially “cooks” the cancerous tissue. In some cases, there is also mechanical damage produced by bubbles (cavitation) generated during the treatment process. A similar approach, known as radiofrequency ablation, uses an oscillating electric field to produce localised heating. Because the surrounding tissue is not exposed to ionising radiation, the side effects are much more tolerable than those produced by radiotherapy. The disadvantage of laser, microwave and radiofrequency ablation is that they all require insertion of a probe to access internal tumours. High intensity focused ultrasound does not suffer from this restriction, but requires long treatment times, although it has recently been applied to the treatment of brain tumours with considerable success [17].
Crucially the 20th Century also saw a revolution in our understanding of biology, with the discovery of DNA and the development of genetics as a scientific discipline. Coupled with equally transformational changes in medical imaging, microscopy and biochemistry, this led to a step change in our understanding of cancer and its progression. This understanding facilitated the development of several new classes of cancer drug [5]. Anti-angiogenic drugs were created to prevent tumours from recruiting their own blood supply and hence starve them of the nutrients they need to survive and grow. Some tumours were found to be highly sensitive to certain hormones, such as oestrogen and testosterone, and drugs to control levels of these hormones have been successfully used to restrict tumour growth. The 1970s and 80s also saw the start of gene therapy which aims to “correct” the damaged DNA and/or replace the faulty genes thought to be responsible for cancer. As mentioned above, the genetic origins of cancer remain poorly understood, but this remains a highly active field of both scientific and clinical research, fuelled by new gene editing techniques such as CRISPR. Genetic profiling of patients is already being used to predict their responses to different treatment regimens enabling these to be personalised.
There were many important developments in mainstream techniques too. Many surgical cancer treatments have been transformed by the introduction of laparoscopic or “keyhole” techniques, which vastly improve safety and recovery times. Developments in reconstructive surgery and prosthetics have also been vital in counteracting the physical and psychological consequences of cancer surgery. Radiotherapy systems have undergone major advances, with the introduction of stereotactic systems that use multiple beams of radiation to focus energy on the tumour whilst minimising damage to the overlying tissue. More recently, FLASH radiotherapy and proton beam systems have been introduced, enabling even higher doses of energy to be delivered with lower risk to the surrounding tissue. The former uses very short, intense pulses of radiation, whilst the latter replaces gamma or x-rays with a beam of protons.
The toxicity of chemotherapy has been mitigated, at least to some extent, by improvements in delivery techniques: e.g., encapsulating drugs in nanoparticles that alter their circulation in the body and are preferentially taken up in tumours; and binding drugs to molecules that specifically target cancer. A final class of drug that should be mentioned in this regard is photodynamic therapy (PDT). These extremely potent drugs remain inert until activated by exposure to light. Provided the light can be adequately focused on the tumour, then the risk of side effects is minimised. PDT has been very successful in the treatment of skin cancer [18]. Two disadvantages are that patients must remain in darkened rooms until the drug has completely cleared from their systems; and internal tumours are difficult to treat due to the need to insert optical fibres through the overlying tissue since light can only penetrate a few millimetres through tissue.
Immunotherapy
Treating Cancer from the Inside
Throughout the history of cancer there have been reports of miraculous cures, spontaneous remissions attributable to the mercy of God or magical influence. The patron saint of cancer, Peregrine Laziosi, was one such survivor, said to have recovered overnight from a cancerous swelling of the leg in 1320. It would take another 600 years for possible explanations of these “miracles” to be proposed, but a recurring feature was that the patients were reported as simultaneously suffering from another disease, often an infection causing inflammation and fever.
These anecdotal reports led to some alarming experiments. In France, physicians deliberately infected patients with dirty dressings from other patients. Breast cancer patients were injected with gangrene and uterine cancer patients with syphilis, the latter on the extremely tenuous grounds that prostitutes were very rarely diagnosed with cancer [19].
Despite the horrifyingly unethical nature of these “trials,” by the late 19th Century, they had attracted considerable interest, including that of a young American surgeon, William Coley. Spurred by a case in his own hospital of a patient mysteriously cured of cancer following a post-operative infection, Coley embarked upon an extensive course of experiments. These eventually led him to formulate a series of “toxins” – bacteria-laden meat broths – which he administered to patients with remarkable success in several cases.
Unfortunately, Coley failed to produce a formal methodology or scientific report of his work, publishing his results only in the form of case studies. Competing with the much more intuitively and commercially attractive radiotherapy [6] and subsequently the boom in chemotherapy, Coley’s toxins were dismissed by mainstream medicine and by 1965 had been consigned to the American Cancer Society’s list of “unproven methods of cancer management” alongside such bizarre remedies as the orgone accumulator, a cabinet in which patients would sit to absorb curative currents of orgone – a universal life force [20]. A further key problem with Coley’s results was that he could provide no explanation as to why some patients experienced complete remission and others simply succumbed to the effects of the infection induced by the toxins. Although vaccination had been introduced to Europe over a century before, understanding of the immune system was still in its infancy. It took several decades and a small number of determined and dedicated individuals [7] to rebut the accusations of quackery and launch immunotherapy into the front line of cancer therapy.
The concept of immunotherapy is comparatively simple and beautifully elegant. The immune system has evolved to protect the body and rid it of disease. Unlike surgery, radiotherapy and even chemotherapy, immune cells can access all parts of the body so can attack both localised and metastatic disease. Moreover, once primed, these cells will stop the cancer from coming back. The workings of the immune system are, however, anything but simple. They are exquisitely complex and are by no means yet fully understood. In order to introduce the multiple types of cancer immunotherapy now being trialled, a brief description of the immune system is needed. Please note, however, that this is a highly abstracted and simplified description, focused on those key elements relevant to cancer immunotherapy.
Fundamental to the functioning of the immune system is a sophisticated network of chemical signals that are exchanged between different types of immune cell and transmitted through the bloodstream and lymphatic system. The chemical composition of a cell’s surface varies according to what type of cell it is and whether it is healthy or diseased. Cells or other entities such as viruses are quickly “recognised” as belonging in the body or not by the immune system due to their different surface chemistry.
Molecules that trigger this recognition are known as antigens. The recognition process may be facilitated by direct interaction between the antigens presented on the cell surface and specialised molecules on the surfaces of immune cells, known as receptors. In the case of foreign cells however, an antigen will typically first be bound by an antibody – a protein molecule with a specific configuration that chemically “locks” to a particular antigen or class of antigens. There are antibodies freely circulating in the blood and lymphatic system as well as on the surface of specialised immune cells. Once attached, the antibody effectively “tags” the antigen enhancing its visibility to immune cell receptors. It is the antibody-antigen combination that then binds to the immune cell receptor.
When a foreign entity is detected, multiple processes may be set in motion, including the activation and proliferation of so-called killer T cells [8]. As its name suggests, when a killer T cell encounters a foreign cell it destroys it, e.g., by releasing chemicals that damage the target cell membrane and/or trigger apoptosis. In principle a cancer cell should look foreign to the immune system as well, just as a dying cell or a cell infected by a virus does. Cancer cells, however, are able to display molecules on their surfaces that allow them to hide from these immune responses. These molecules achieve this by binding to specific receptors on the T cells which prevents them from being activated. Essentially the cancer cells hijack the mechanism that healthy body cells use to prevent accidental triggering of the immune system against normal healthy cells. These are known as immune check points.
There are multiple approaches to cancer immunotherapy being trialed and even more under intense research. One of the earliest and arguably the most successful to date is to use synthetic antibodies that bind to receptors on certain types of cancer cells and stimulate an immune response. The breast cancer drug, Herceptin (Trastuzumab) developed by Genentech in the 1990s is a famous example.
An even earlier approach was to synthesise one of the chemical messenger molecules or cytokines secreted by immune cells to stimulate the activation and proliferation of T cells. Although initially investigated as a combination product with adoptive T cell therapy (see below), interleukin 2 or IL2, is now approved as a standalone drug for kidney cancer. Another cytokine, Interferon is also approved for leukaemia and lymphoma treatment.
A key strategy in cancer immunotherapy is checkpoint inhibition. Antibodies that block the receptors that deactivate the T cells are administered so that immune cell mediated destruction of cancer cells can proceed. The key underpinning science was developed by James P. Allison and Tasuku Honjo who shared the 2018 Nobel prize for their work. The first check point inhibitor to be trialed – anti-CTLA4 or Ipilimumab- was found be highly effective, indeed curative in some patients but also caused very severe side effects due to the unregulated immune response. An alternative strategy is to block the molecule on the cancer cells that deactivates the T cell. This is the basis on which anti-PDL1 drugs work. Trials are ongoing but the localisation of the immune response to cancer cells appears to lessen the risk of dangerous side effects.
Complementary to checkpoint inhibition are cellular therapies. In Adoptive T Cell Therapy, T cells that have already been primed by exposure to cancer cells are extracted from patients and replicated outside the body. The resulting army of T cells is then reinjected. Chimeric antigen receptor (CAR) T Cell Therapy uses a similar principle, but the T cells are primed by genetically engineering them to express the appropriate cancer specific receptor. In Dendritic Cell Therapy a different type of immune cell, dendritic cells, are extracted and primed by exposing them to tumour tissue antigens. When reinjected, the dendritic cells “present” the cancer specific antigens to T cells in order to stimulate them to attack. The success of cellular therapies has so far been primarily in blood borne cancers, but numerous trials are currently underway, including in combination with check point inhibitors.
A further class of immunotherapy uses genetically engineered “oncolytic” viruses that selectively infect and kill cancer cells. The advantage of viruses over conventional drugs is that they are self-sustaining i.e. they will continue to replicate inside the tumour, infecting and killing malignant cells until there are none left. To date the success of oncolytic viruses has been limited to certain types of tumours. One challenge is that the immune cells that fail to attack the tumour cells will unfortunately inhibit the spread of the virus. It is possible that this may be overcome by combining viruses with checkpoint inhibitors.
The Future?
We’re Not There Yet
The last 100 years, indeed the last 10 years, have transformed the outlook for many cancer sufferers and the future looks even more hopeful. A note of caution is nevertheless appropriate. As the above discussion has shown, the history of cancer therapy is filled with examples of premature optimism and a 15% improvement in death rate, whilst very encouraging, is a long way from elimination of the disease.
Moreover, progress has been extremely uneven across different types of cancer. For many forms of breast, prostate and blood cancer, survival rates have improved dramatically in the last 50 years. In stark contrast, for aggressive tumours such as glioblastoma multiforme in the brain and pancreatic adenocarcinoma, there has been little improvement in survival since the 1960s. A repeated and frustrating finding is that treatments that work spectacularly well in one type of tumour in one patient may fail completely in another. This is as true for modern immunotherapy drugs as for early chemo and radiotherapy treatments.
There remains a plethora of open questions. For example:
- Scientific - as mentioned above, the fundamental mechanisms via which cells become malignant have yet to be fully understood. We still do not know why some individuals develop cancer when others with apparently similar genetic characteristics and lifestyles remain cancer free. The relationship between cancer and the immune system is also only just starting to be unravelled.
- Ethical - there has been an explosion in the number of clinical trials for new therapies, but it will take many years to establish which are effective, in which types of cancer, in which subset of patients. Should cancer patients have the “right to try” experimental techniques, or do we need even tighter regulation? Similarly, techniques for genetic engineering are evolving at a rapid pace, offering tremendous potential benefits in certain types of cancer but equally raising important ethical concerns over their long-term consequences and/or misuse.
- Economic - the cost of many new therapies is enormous. For example, the cost of a single course of immunotherapy can easily exceed £100,000 (~10 times the cost of a standard course of chemotherapy). This poses a major challenge for healthcare providers, even in developed countries, and puts novel therapies out of the reach of many patients worldwide.
- Political - as we gather more and more data indicating correlations between certain types of cancer and environmental pollutants, drugs and foodstuffs, should we legislate to ban certain substances?
Prevention is Better Than Cure
A vital point to make is that the success of many cancer treatments has been due not only to improvements in the treatments themselves, but also to improvements in screening processes enabling earlier diagnosis and intervention. As imaging and other analytical techniques become more and more advanced, this will hopefully lead to even more timely and effective treatments.
Similarly, vaccination and sanitation are widely recognised as two of the most impactful developments in public health, largely responsible for the significant fall in deaths due to infectious diseases and our increased life span. A universal vaccine for cancer is sadly unlikely but increasing our focus on preventative measures could yield enormous benefits both clinically and economically. It is estimated that the roll out of human papillomavirus (HPV) vaccines which started in 2006 may prevent up to 90% of specific types of cancer (cervical, anal, oropharangeal and vaginal) [21]. Even simpler measures such as changes to diet, activity levels and sleep quality are also being shown to have a positive impact on the risk of developing many cancers [22]. As our scientific understanding increases, the role of prevention may even overshadow that of treatment.
© Professor Stride 2022
References & Further Reading
References
[1] British Broadcasting Corporation News. https://www.bbc.co.uk/news/health-31096218
[2] Roser, M “Progress against cancer.” Our World in Data 2020 https://ourworldindata.org/progress-against-cancer
[3] Roser, M et al. "Life Expectancy". Our World in Data 2013 https://ourworldindata.org/life-expectancy
[4] Hanahan, D & Weinberg, R. "The Hallmarks of Cancer". Cell 2000, 100, pp 57–70.
[5] Hanahan, D & Weinberg, R. "The Hallmarks of Cancer: The Next Generation ". Cell 2011, 144, pp 646–674.
[6] The Science of Cancer (2017) a collection published by Scientific American. ebook available at: https://www.scientificamerican.com/store/ebooks/the-science-of-cancer/
[7] Shultz, M, et al. “Oldest known case of metastasizing prostate carcinoma diagnosed in the skeleton of a 2,700-year old Scythian king from Arzhan (Siberia, Russia).” International Journal of Cancer 2007, 121, pp 2591–5.
[8] Zink, A, et al. “Malignant tumors in an ancient Egyptian population.” Anticancer Research 1999, 19, pp 4273-7.
[9] Odes, E, et al. “Earliest hominin cancer: 1.7-million-year old osteosarcoma from Swartkrans Cave, South Africa.” South African Journal of Science 2016 article 2015-0471.
[10] Seper Ekhtiari, S, et al. “First case of osteosarcoma in a dinosaur: a multimodal diagnosis.” The Lancet Oncology 2020, 21, pp1021-1022.
[11] Mitchell, P, et al. “The prevalence of cancer in Britain before industrialization.” Cancer 2021, 127, pp3054-3059.
[12] The Smith Papyrus: translation available at: https://oi.uchicago.edu/research/publications/oip/edwin-smith-surgical-papyrus-volume-1-hieroglyphic-transliteration
[13] The Ebers Papyrus: translation available at: https://web.archive.org/web/20130921055114/http://oilib.uchicago.edu/books/bryan_the_papyrus_ebers_1930.pdf
14] Hippocrates, Hippocratic writings. Edited with an introduction by G.E.R. Lloyd. Harmondsworth (Penguin), 1978, 236.
[15] Mukherjee, S. The Emperor of all Maladies: A biography of cancer. New York: Scribner. 2010.
[16] Mould, R. “Emil Herman Grubbé (1875–1960) with special reference to priority for X-ray cancer therapy.” Journal of Oncology 2018, 68, pp 286–289.
[17] Carpentier, A. “Clinical trial of blood-brain barrier disruption by pulsed ultrasound.” Science Translational Medicine 2016, 8, pp 343-353.
[18] National Institutes for Health “Photodynamic Therapy.” https://www.cancer.gov/about-cancer/treatment/types/photodynamic-therapy
[19] Graeber, C. The Breakthrough: immunotherapy and the race to cure cancer. Scribe. 2018.
[20] British Broadcasting Corporation News. https://www.bbc.com/culture/article/20210426-the-man-who-thought-orgasms-could-save-the-world
[21] National Institutes for Health “HPV Vaccines.” https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet
[22] Sanchis-Gomar, F, et al. “Physical Inactivity and Low Fitness Deserve More Attention to Alter Cancer Risk and Prognosis.” Cancer Prevention Research 2015, 8, pp 105-110.
Further reading
The Science of Cancer (2017) a collection published by Scientific American. Ebook available at: https://www.scientificamerican.com/store/ebooks/the-science-of-cancer/
Mukherjee, S. (2010). The emperor of all maladies: A biography of cancer. New York: Scribner.
Graeber, C. (2018) The Breakthrough: immunotherapy and the race to cure cancer. Scribe.
Hajdu, S. “A note from history: Landmarks in history of cancer.” Cancer 2011, 117, pp 1097-1102.
https://researchbriefings.files.parliament.uk/documents/SN06887/SN06887.pdf
https://raconteur.uberflip.com/i/521961-cancer-treatments/5?
Suggested Visits
The Science Museum Wellcome Galleries, South Kensington, London https://www.sciencemuseum.org.uk/see-and-do/medicine-wellcome-galleries
Petrie Museum, University College London, https://www.ucl.ac.uk/culture/petrie-museum
Hunterian Museum, Lincoln’s Inn Fields, London, https://www.rcseng.ac.uk/museums-and-archives/hunterian-museum/
The Wellcome Collection, Bloomsbury, London, https://wellcomecollection.org/
[1] in the case of cancers such as leukaemia the proliferation of cancerous cells occurs within the blood stream rather than forming a solid mass.
[2] It should be noted that some of the herbs used by ancient and mediaeval physicians did become the basis for modern chemotherapy drugs and opiates are still widely used for pain relief.
[3] Ironically, however, it was the failure of sterile technique that provided a crucial clue that would later unlock a completely different approach to cancer therapy.
[4] This included work on early cancer “vaccines”
[5] The term drug is used here in its widest sense to describe a substance that produces an effect on the body as opposed to a simple chemical.
[6] It cannot have helped that one of the major benefactors of the hospital in which Coley worked was a mine owner supplying the hospital with radium [19]
[7] These included clinicians such as Steven Rosenberg who were captivated by their own direct observations of patients and Coley’s daughter who though not a clinician or a scientist was convinced of the credibility of her Father’s results. She diligently assembled his notes and set up the Cancer Research Institute.
[8] T refers to the Thymus gland where T cells mature
Further reading
The Science of Cancer (2017) a collection published by Scientific American. Ebook available at: https://www.scientificamerican.com/store/ebooks/the-science-of-cancer/
Mukherjee, S. (2010). The emperor of all maladies: A biography of cancer. New York: Scribner.
Graeber, C. (2018) The Breakthrough: immunotherapy and the race to cure cancer. Scribe.
Hajdu, S. “A note from history: Landmarks in history of cancer.” Cancer 2011, 117, pp 1097-1102.
https://researchbriefings.files.parliament.uk/documents/SN06887/SN06887.pdf
https://raconteur.uberflip.com/i/521961-cancer-treatments/5?
Suggested Visits
The Science Museum Wellcome Galleries, South Kensington, London https://www.sciencemuseum.org.uk/see-and-do/medicine-wellcome-galleries
Petrie Museum, University College London, https://www.ucl.ac.uk/culture/petrie-museum
Hunterian Museum, Lincoln’s Inn Fields, London, https://www.rcseng.ac.uk/museums-and-archives/hunterian-museum/
The Wellcome Collection, Bloomsbury, London, https://wellcomecollection.org/
This event was on Wed, 16 Feb 2022
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login