The Stigma of Mental Illness: Inevitable or unjustifiable?
Share
- Details
- Text
- Audio
- Downloads
- Extra Reading
Stigma and discrimination against people with mental illness is common and severe wherever it has been studied. One surprising aspect of this is that many consumers report that they feel discriminated against by health and social care staff, even though these are precisely the staff who are trained and experienced in offering assistance to people with mental illnesses. Furthermore, the 'social contact' hypothesis suggests that those with more contact with people with a diagnosis of mental illness will have more favourable and less stigmatising views. This lecture will review evidence about discrimination and evidence of what is effective to reduce stigma and discrimination.
Download Text
THE STIGMA OF MENTAL ILLNESS:
INEVITABLE OR UNJUSTIFIABLE?
Professor Graham Thornicroft
My topic today is about stigma or, more precisely, about stigma and discrimination. I am going to talk to you about why I think this is common, often serious, and also what we may be able to do about it.
Part of what I am going to say is a summary of a book I did a couple of years ago called Shunned, published by Oxford University Press. I am going to begin by summarising some of the evidence that discrimination and stigma are actually common and often intense.
To write this book, I started by reading everything I could about stigma, not just about mental illness, also about intellectual impairment, people of short stature, people with facial disfigurement, sex workers - there is a whole range of publications about stigma. Then I also wrote to people I was treating in Croydon, in South London, and I said if you have felt or been discriminated again, I would like to know about it - can you please tell me, write to me with the details. Some people wrote a sentence or two, some people wrote a paragraph or two, some people wrote chapters, with massive amounts of detail, about their experience of discrimination. From that, I came to think that there is actually something very important here that is really not been addressed, certainly by the research world, and so I set up a group of colleagues, across many countries, to look into this in more detail.
I came, quite early on, to the conclusion that stigma itself is a type of overarching term, but it is actually very imprecise, and the world has not made big strides so far in terms of making any impact to reduce stigma and discrimination. I have come to the view it is actually more helpful to see stigma as this overarching term that in fact contains three more specific challenges. The first is the problem of knowledge, namely most of what we all think and know about mental illness is actually very limited, and much of the knowledge people have is actually wrong, so it is a mixture of ignorance and misinformation. Secondly are the feelings and the emotions that go around, partly from, if you like, the wider host community towards people with mental illness, but also from people with mental illness towards themselves and to other people with mental health problems as well, and that's prejudice. The third challenge is one of behaviour: namely, if I apply for a job, and if I disclose that I have had a mental health problem, am I even going to be short-listed or not - probably not - and it's the behavioural area that I call discrimination. I am going to be focusing today especially on discrimination because I think this is the most important of these three domains.
For example, my mother was a district nurse for 20 years, then she gave birth to my sister, and she had a severe period of postnatal depression. It was so bad that she was off work for a year, she needed some electroshock therapy, and then she got fully better. I said to her recently, 'Mum, when you went back to work, what did you say to your boss? Did you disclose that you had a mental illness?' She said, 'Of course not! Are you daft?!' because she felt then, and this is 50 years ago, that had she disclosed, probably she wouldn't have got her job back, and I think she's probably right, and I also don't think the situation has changed very much, at least in the NHS, unto this day.
I have an example about some of the ways that children, for example, respond towards the mental illness theme. We did a study of a couple of hundred kids in Kent, 14-year old schoolchildren, and they didn't want to have anything to do with a session about mental illness. So we had a warm-up session, and we said, 'Just shout out words that you have heard used to refer to people with mental health problems.' The most frequently occurring words were: disturbed, nuts, confused, psycho, spastic, crazy, depression, disabled, mad, unpredictable, insane, loony, and so on. They came up, to our amazement, with 250 different words or terms, and then we went through and categorised them, and 70% were negative and 30% were neutral and nil were positive. So that is an indication about the sort of feelings within just the young community about the mental illness theme.
A large proportion of the things that people write about mental illness are related to violence, threat, and unpredictability. An amazing amount of the literature on stigma is about people with schizophrenia, and you search almost in vain for anything about people with anxiety disorders, panic attacks, phobias, even not much about depression. There is very little attention to people's feelings towards mental illness, and almost nothing known, at least in the scientific literature, about discrimination, about behaviour, particularly behaviours that limit participation and social inclusion and full citizenship for people who disclose having mental health problems. There is almost nothing written by people with mental illness. The papers you read act as if people with mental illness are not able to speak directly on their own behalf, and there are very few intervention studies to see what might actually make a difference; rather the opposite: a lot of papers seem to be based on the assumption that stigma is very difficult, it's almost tribal, it's somehow intrinsic, there is sort of 'us', there's an in-group, there's the other, and it is somehow a part of human society and you cannot change it, none of which I agree with, but there is a rather pessimistic feel when you read this type of material.
From my reading of the literature, from what people I have been treating tell me, I am going to go through some of the evidence that discrimination does take place and can have profound implications.
Let us start in the home. There is a lot of material now to say that when somebody, perhaps a young person, first develops the features of a mental illness - for example, they might go out to college or to work, they may be staying in bed, maybe not eating so much - then initially often the family use moral explanations. They will accuse the person of lacking in moral fibre, not enough 'get up and go', accuse them of being lazy or weak. Once the person has received treatment and probably a diagnosis, there is another facet, namely that the family members also feel stigmatised against. Suddenly, you find that other family don't visit so much, or you are not invited out to social occasions as much as you had been. That is sometimes called stigma by association, having impacts also upon wider family members, and in some cultures, for example in South East Asia, also a sense of embarrassment and shame upon the whole family, not just the person concerned. We also know that there are higher rates of insecure accommodation and also homelessness among people especially with psychotic disorders, and we know as well that, in many areas, there are profoundly unwelcoming reactions when there are plans to accommodate people with mental illness in the neighbourhood.
For example, there was, an old people's home in Yorkshire, and there was a plan to make it into a residential care home for people with mental health problems. Typically, out came a number of neighbours, mostly young mothers with their children, and they were protesting, and they had placards and they had petitions and they went to the town hall, and they visited the planning committee and so on to try and stop this. Now, from my own clinical background, I have been through similar occasions five times, setting up local community care centres, and every time, we had the same type of reaction, and I wasn't always best pleased to meet with this type of reaction from neighbours, but in fact, thinking about this more, I have changed my mind, and I think that what people like this are doing is entirely reasonable. It is entirely reasonable based upon the knowledge and the information that they have, and the information they have mostly says people with mental illness are a threat, you certainly don't want them living next door to you, and they are a threat to your children. So it is not that the people are malevolent; it is that the information they have is extremely thin on the ground, it is very partial, and it is almost entirely negative.
The second domain is in terms of close relationships, friendships and also intimate partnerships. From the work I have been doing in the last couple of years, it is remarkably common, and I have been a psychiatrist for 20 years, but still I have been surprised to find how often friends especially, sometimes family members, distance themselves, quite often cut off all contact, and repeatedly we hear of young people, for example, developing a psychosis who lose all their friends very rapidly after the onset of the condition. One implication of that can be limited or impaired or casualised sexual relationships; it is very difficult to keep an ongoing relationship persisting.
Surprisingly commonly, to me at least, many people report losing many or all of their friends when a condition starts. Oddly enough as well, often people say, 'I couldn't have predicted who would stand by me and who would abandon me.' Sometimes acquaintances suddenly came true and were a rock, and then closest friends disappeared entirely and very rapidly.
An area where there is quite a lot of evidence of adverse implications of having mental illness is within the job market. There is pretty good evidence for all of these: that you are less likely to be short-listed or hired if the interviewer knows you have a mental illness; more often made redundant; lower rates of pay; poorer promotion prospects; and what this adds up to is the terrible dilemma for someone who has a mental illness about whether to disclose or not. As things stand, it's a no-win situation because: if you do disclose, then you will usually have a lower chance of getting even short-listed, let alone getting the job, but, if you get the job, then you can claim all the entitlements under the Disability Discrimination Act in this country; if you don't disclose, then you might have the feeling you have got to remain eternally vigilant - you certainly could not be seen to be taking a tablet, you cannot easily have time off to go to an appointment because you could not declare what it was for, and you fear that if you are found out, you might lose your job or be punished somehow. So it is very difficult to know right now just what to do if you have, or if you have had, even years ago, a mental health problem, when it comes to making a job application. In fact, we are doing work on this at the moment, and it looks to us like the legal requirements to disclose anything, for the vast majority of jobs, are nil; that legally you have to disclose very little indeed about a mental illness when you are applying for a job at that time.
I think it is important to appreciate the severity of these implications. There are data from the Labour Force Survey, official Government data, and they show the proportion of people in different categories actively working. At the top are all adults in the population, 75-80% or so; people with long-term physical disorders are nearly 60%; and people with longer term mental illnesses, about 15%. If you are talking about where I work, in South London, and if you think about people with bipolar disorder or schizophrenia, then it is about 5% of such people have work on an ongoing basis, even part-time work. So in effect, it is the inverse: it is 70-80% in work for people with physical in the general population; it is about 70-80% out of work if you have a long-term mental disorder. Not all of that is simply because of the impairments from the condition itself. If you look at Spain or Italy, for example, you can easily get double the rates, 20-30%, of very similar people who actually have paid work on a regular basis, so some of this is because of the context in which we structurally exclude such people from the job market.
There is a charity called the Shaw Trust. I had never heard of them till two years ago, when they brought out a remarkable report. They did a survey of 500 bosses of companies all over the country, and they asked them lots of questions about mental health, and one of them was, 'What percentage of people in your organisation will have a mental health problem in their lifetime?'
Now, this the brief audience participation element: who would like to suggest a number? The proportion of people, let's say in a company, who will have a mental health problem at any time in their working life - what do you think the answer was?
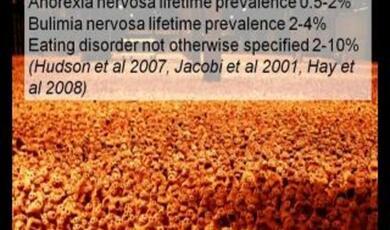
If it's 'lifetime ever', is the jargon, meaning throughout your adult life, what's the proportion, it is a half, 50% of us, of everybody. If it is this year, the answer would be 25%. So when you say to bosses, 'How many of your workforce do you think are going to have a mental health problem in their working lifetimes?' the answer would be about 50%. In fact, half of them said nil. So this comes back to my point about information, the challenge of ignorance. It is not that those bosses are necessarily going to be unsympathetic, or deliberately malevolent; they actually don't understand the issues at all. They have no idea how common these problems are, and what are the features, and what they should do. They did not know the Disability Discrimination Act does apply to people with all disabilities, including those which are mental health related.
The other area in which there is lots of material to report, and I'll summarise today, is about the media. To boil it down, if you take, for example, analyses of press cuttings, and then you say, well, this is favourable, unfavourable, and so on, you find that about between a third and two-thirds - it depends on the paper or the journal or the magazine - of all the articles are focusing on risk and violence. The medium which is by far the most hostile are children's cartoons, animations, like Disney - think of Looney Tunes, for example - where up to 85% of all the characters identified as having a mental health problem are a threat, are unpredictable, are not like the host community. What you also find in the, let's say, magazines and newspapers, until very recently, is very few direct quotations from people with a mental health problem. There is also lots of evidence now, for example a series of surveys in Greece and in Germany, that what happens in the media does have an effect upon the public opinion. So we are used to this now. I have actually been part, with some charities, of going to the Press Complaints Commission, and the rule for 'schizo' is that you should not use it to address an individually named person, but the PCC does allow use of the 'schizo' word to apply to a category or to a group of people, so we have some very odd rulings about these grossly pejorative terms. It is also common to see headlines where there is no evidence presented whatsoever that the perpetrator of a crime, or the alleged perpetrator, has any mental health problem, but they are nevertheless described as 'manic' and 'schizo' and so on.
The Government has an anti-stigma initiative called Shift, and a couple of years ago they did an analysis of what we found in lots of newspapers; some national papers, some local. One of the interesting things was the most frequently reported topics. The thing I want to draw your attention to is that, by quite a long way, the most frequently reported topic for all mental health stories is homicides, and then you have drugs, depression, wellbeing and so on, and anything to do with services or care, which are about 5% or fewer, so it is very clear what newspapers like to report: they like to report dramatic and serious crime.
I mentioned when I began that, from looking into this in some detail, I came to the conclusion that, under the whole heading of stigma, I think the most important thing is discrimination. So if, for example, I find my various responsibilities too much, and I become depressed one day, and I have to take some time off work, when I am ready to go back to work, and I go to my boss, I don't really think, I don't care what my boss knows about mental illness. Now, working in the Institute of Psychiatry, I would hope it is quite a lot, but I don't really care what he thinks about it. I don't really care what he feels about people with mental illness either. What I really care about is his behaviour - is he going to give me back my job or not. Interestingly, some of our recent research is suggesting that the knowledge and the attitudes and the behaviour are probably, to some extent, separate elements, and simply teaching the public about mental illness will not necessarily have an impact upon anybody's behaviour.
So we have decided to go ahead and start a lot of research on this. We have got a group now of countries all over the world, doing research on discriminations and what are people's experiences. The first study I can tell you a bit about. It refers to people with schizophrenia. We wanted to develop a way to assess, directly from the reports of people with mental illness, their experience of discrimination, and the scale is called DISC. We wanted to know what types of discrimination occur, what parts of lives it has an impact upon, and also how common and how severe it is. So we asked, for example, some of the things I mentioned earlier, about the impact upon housing, upon personal relationships, upon work, upon marriage, childcare, involvement in social clubs and leisure, privacy, safety, all sorts of issues, and I want to tell you a little bit about it.
The first study we have done was carried out across 27 countries around the world, with over 700 people being directly interviewed. For example, there was a team of collaborators working in a charitable group in Lithuania. The first thing we said was: 'Tell us in what ways you have experienced discrimination because of your mental health problem.' A lot of people said, well, simply having the diagnosis of schizophrenia itself was a disadvantage. In fact, in some countries, it is still common for the doctors not to give that word because it is seen as so toxic, and if they are given that word, in a lot of countries, people receiving it have at least profound ambivalence, if not a very strong aversion, to labelling themselves in that way.
Almost half the people reported problems in friendships. Discrimination by the family as well - I mentioned earlier the moral or the weakness or the laziness idea, but also, there can be ongoing resentment by family members: for example, that young person isn't developing their career or their education as the family had originally hoped. Relationships with neighbours also quite common, and other things about work also important.
One of the background questions is: are stigma discriminations basically similar in different countries, in different cultures, or different? There has been really very little information about this until the last year or two. Our results are suggesting that there are largely similar amounts or degrees of stigma across many countries that we have studied.
As we developed this scale, we started by saying 'Have you had discrimination in applying for a job? Have you had discrimination in terms of your friendships?' with the idea that the person with mental health problems was almost, if you like, the victim or that there was incoming almost missiles of discriminations, but it became clear quite quickly that that is a grossly over-simplistic view, and that a lot of people who have mental health problems learn, in a sense, to discriminate against themselves. Sometimes this is called self-stigma. I think it is quite helpful to see this as anticipated discrimination.
I will give you an example. I interviewed a man in Camberwell, a man of about 40, who has had schizophrenia for about seven years. I said to him, 'Have you been discriminated against in applying for a job since you developed your mental illness?' He said, 'No.' He said no a little bit too quickly, so I was suspicious, so I said, 'Well, since you have developed your mental illness, have you actually applied for any jobs?' He said, 'No.' So I said, 'Why not?' and then he came out with this phrase, he said, 'Everybody knows that people like me can never work again.' So I said, 'That's a very interesting statement - can you tell me why you say that?' He said, 'I'm schizophrenic, and schizophrenics can't work.' So he had a very clear view, and he had not been discriminated against by anybody else because he actually had not applied, he had not put himself in the position to be discriminated against; he had almost got his discrimination in first, so his attitude was, why try?
It is clear that part of the reason for these very low employment rates is because of actual discrimination, at application or at interview, but also a large part is because many people with mental illnesses either don't apply at all for jobs or, after some failures, quickly learn not to bother wasting everybody's time in doing so. We have been able to measure this as well. For example, we found that over two-thirds of these 700 people around the world have deliberately wanted to conceal their diagnosis. Two-thirds, again, have anticipated discrimination when applying for a job, and over a half in looking for a close relationships, and two-thirds in some other domain - it might be somebody is, perhaps, an avid footballer, but drops out of a team when they develop a mental illness because they think they are going to be ribbed and mocked. Maybe somebody is in a choir, or whatever it would be, but they actually drop out because they expect embarrassment or ridicule. Again, we wanted to know whether these anticipations are different in different countries, and effectively found very little. We found largely a consistent picture across South East Asia, across the whole of Europe, North America, South America - very similar degrees of expectations of discrimination around the world.
We then wanted to find out, if a person is not applying for a job, is that because they have had rejection repeatedly and stopped, or because they never applied at all? So we asked: 'In applying for and finding a job, or finding work, did you experience discrimination but not anticipate it?' About a third experienced it and anticipated it. Relatively few neither experienced nor anticipated, but the biggest category was people who did not experience any discrimination but did anticipate it. So the most frequently occurring reason for people having this distance from being able to apply for work is because they stop themselves from doing so. So if we think that all you have to do is to teach employers to be fair employers and to act in accordance with the Disability Discrimination Act, that is not the whole picture, because they will not be interviewing people who are choosing not to apply in the first case.
So in a sense, if we have a person with a mental illness or a mental health problem, there would be all sorts of incoming discrimination from the outside world, and we could take measures such as anti-discrimination laws to minimise or even, over time, to eradicate that; but, at the same time, we need to be aware of the anticipated discrimination within the person with the mental health problems. It is plausible that we need to think about forms of empowerment or resilience-building which allow that person to make the application, maybe to make repeated applications, until such point that they get some success in getting a job, and then build on that through references to re-establishing a career.
So, what I have said so far is to argue that forms of discrimination can be far-reaching, and also that they can have serious impacts upon people's lives, effectively to exclude them from social participation, some forms of basic human rights and citizenship as well, but also particularly to exclude them from the workplace.
In the next section, I want to say something about how we might go ahead and reduce discrimination, and I want to talk about two things: actions that can be taken locally; and actions that we can take nationally.
Let's start with the local ones. The basic idea is very simple and very clear, and it is called the Social Contact Theory. We can think about Princess Diana going on television and shaking the hand of a person who is HIV positive, showing the nation that you can touch somebody, you don't catch it immediately, here I am having direct personal contact. Well, the idea works in mental health as well. One of the most powerful ways to reduce stigma is to have direct contact with somebody who is particularly, for example, in a teaching role - somebody like me today - who is talking about two things: talking about the condition - what are the symptoms, how does it affect, how does it start; and talking about their experience of contact with the mental health system, both good and bad.
I had an e-mail this morning from a colleague in Scotland, who has written a book about her experience of having bipolar disorder. She has actually been in hospital for a large part of last year. I was expecting her to talk about the catalogue of unfortunate aspects of treatment. In fact, she did not. She, in detailed accounts, said how marvellous the staff had been, and how effectively they have saved her life through these last months. So the treatment is often experienced as either profoundly supportive or welcoming, or, quite often, as aversive and coercive as well.
The idea is that, within groups, let us say a small group like this, a person with mental illness is in the teaching role, and that can have a very beneficial effect to reduce stigma. We have tested this. We have gone to different groups in London and in Kent. We have worked closely with a charity called Rethink, and they do the teaching and, as the scientists, we do the assessment to look at the impact of it, and we have now done it with three different groups: with police officers, with school children, and with medical students. We are now doing it as well with trainee psychiatrists and with trainee nurses, and soon we are going to be doing it as well with trainee teachers. The basic finding is a very simple one, which is that we can get big improvements in knowledge and attitudes quite quickly through those simple teaching techniques.
One of the most striking findings was from our contact with the police officers. There were about, as I recall, 90 police officers in Kent, and it was one of their in-course, continuing professional development sessions, and the active agreement were two people with mental health problems talking about the condition and about their treatment. Immediately after the teaching sessions, we said, you, you police officers: 'What did you find was especially helpful? Was it (a) the talks of the service users, (b) the facts - we had little cards to put in their wallets, information sheets, or was it (c) a role play? The police had to role play, which was them in a public place, meeting a person acting as if mentally unwell, and taking that person to a place of safety, something police do quite often. 10% of them said said what the patients had to say was not very interesting; some said they liked the facts; and others said they thought the role play was quite good.'
We went back, a month after the teaching session, and said, 'Hello, remember us? We've come back again! Think back now to those teaching sessions and tell us what was actually useful to you.' Then nearly a half of them said, 'Oh, what that patient had to say, that was quite interesting - I had never thought about it from their point of view. Their perspective was quite interesting, you know, and those handcuffs, I didn't realise that people found that so unpleasant.' The facts disappeared, only 5% responded positively, absolutely useless - all these numbers and percentages and statistics, they all forgot it! The other, the interactive element, the other role play thing, was still maintained by about a third. This strongly supports the so-called Social Contact idea: that it is the direct communication from people with mental illness that can make the difference.
Briefly, I will go on to say a bit about what can be done at the national level. We have growing information about this because of campaigns conducted in Australia, and in Scotland, and New Zealand, and a campaign about to start in this country. I will show you an example from New Zealand's national TV campaigns that they have run over the last few years.
Who's heard of John Kirwan? Anybody? He was the captain of the New Zealand Rugby Union team 10 years ago, so a national icon. He typifies sort of macho strength and muscular virility, so it was a sensation when he came out on national television in New Zealand to say that he'd suffered from depression and had treatment and recovered in that way. He was the leading figure, for a couple of years of the campaign, in the depression part of the anti-stigma campaign. Seventy-eight per cent of the country saw that advert with John Kirwan, and of those who saw it, 98% were positive about it, and they particularly remarked upon his honesty and his integrity and the positive way he talked about having mental health problems. For a couple of seasons, they actually featured celebrities in that way, to get out into the public domain the message that these are common problems, they are treatable, and it is not shameful to talk about having it, or having had it.
Does doing that actually make any difference? We have the results of surveys in New Zealand over four different years, and there is lots more information like this. The ststement 'People nowadays are more accepting of mental illness,' went up from 43 to 55%, so at least 10 points' increase over that period. The statement, 'People with mental illness can still lead normal lives,' went up from 72 to 82%, from this national survey of population. 'Mental illness can happen to anyone,' rose from 87% to 93%. This shows, for example, that those people who say, 'Stigma, it's all very difficult, you can't change it,' are wrong; you actually can change it, and you can change it in a positive direction.
When I wrote a book a couple of years ago, I read a very large amount of pretty miserable material about these issues, and I asked myself, 'Are we seeing any favourable change?' and certainly as of two years ago, I could not honestly say that society was tackling stigma any better now than it was decades ago, but I am beginning to see signs that there is a type of sea-change beginning within our own country.
Kelly Holmes, our golden girl, who won two Gold Medals in Athens, disclosed that, when she was training, she thought that she would not be able to compete because she had a serious injury, and at that time, she started to cut her abdomen with a razor. She was quite open about this, after coming back as a double Olympic Gold Medal winner.
Also in the sports domain, Frank Bruno disclosed that, during a period of most intense personal difficulty, he, perhaps related to cocaine, had developed what was diagnosed as a bipolar disorder and in fact was detained under the Mental Health Act. I recall this very well. I was driving home one day, and there was a reporter saying, in sort of solemn tones, 'Friends and relatives are enormously sad to hear this about Frank, this terrible news,' and I thought, 'Oh my goodness - he has died!' and then they said, '...the news that he has been sectioned in a mental hospital,' and I thought, 'Well, it's not that bad!' but it is treated as an enormous calamity in his life. In fact, he has written an autobiography since then about it.
One man who was the captain of Celtic and national hero in parts of Scotland - not among Rangers fans of course! - and before he retired, he had a large spread in the Daily Record saying that he had been taking antidepressants for many years and having periods of great difficulty, which had not actually interfered with his play, but difficulty because of depression.
Another footballing hero is Paul McGrath, who used to play for my own team, Aston Villa - he's a hero in the South of Ireland, and also used to play for Manchester United. He has written a book, again disclosing about his periods of mood swings, his severe alcohol dependence, and also periods of self-harm.
A footballer called Mark Yanson had a severe scooter accident (maybe it was a moped), and after that, was physically injured and also developed a severe depression, and now writes about this in his own right.
Stephen Fry has also made an important contribution to our understanding about the nature of bipolar disorder, and also, he drew in Richard Dreyfuss and a number of other celebrities, showing that you can live a successful life and also have, in some cases, severe mental health problems at the same time.
Bill Oddie talked about his depression, and also about the fact that his mother was in an institution for many years. Some of you may recall him as a member of the Goodies, a comedy group, and more recently as a famous twitcher or birdwatcher and naturalist. Nevertheless, although he plays a chirpie on the box, he has periods still of serious depression.
How many people can name a man serving as an officer or Minister of Government who, while in office, has disclosed having a mental illness? Does anybody know any names?
I can think of only one, and it wasn't John Prescott, because he wrote his autobiography just after leaving office, and what was picked up, among hundreds of pages, was the fact that he had behaviour that was possibly bulimic; and it was not David Blunkett, because he also disclosed his periods of depression after leaving office, and that in fact that throughout most of the 10 years while he was a Cabinet Minister, he had been treated for depression.
It was Kjell Magne Bondevik. This is a remarkable man. In 1998, he was the Prime Minister of Norway. He woke up one morning and said, 'I can't get out of bed.' He called in his Deputy Prime Minister and said, 'I'm very sorry, Deputy Prime Minister, but I can't get out of bed, I have a mental problem - you will have to run the country.' The Deputy Prime Minister said, 'Oh my goodness, oh my goodness, Prime Minister, what shall we tell the people?!' To his eternal credit, Mr Bondevik said, 'We shall tell it as it is.' So the Deputy Prime Minister went on the television and said, 'I am very sorry, the Prime Minister has depression, and he is receiving treatment, and he will be back as soon as he can. Meanwhile, I am in charge.' Just over a month later, Mr Bondevik came back and resumed office, carried on, and I think the most remarkable part of the story is that, two years later, he stood again for election, 2000 it would have been, and he won.
Just before I finish, a note about what you can expect next year. In a remarkable investment, the big lottery fund has given 16 million and Comic Relief has added 2 million to start a new programme to reduce stigma and discrimination in England, and this is called 'Time to Change'. It is a campaign with four organisations working in partnership, which is Mental Health Media, Mind, Rethink, and our own team at King's College London, as the so-called evaluation partner. We are going to be measuring whether this works or not. The main campaign on television will be starting next January, and then you will I hope be seeing waves each year for the next four years. I expect we will not be able to get rid of stigma in four years, so we actually need to take I think, to begin with, a 10 year prospect, if we are serious about making an impact. We have already done some pilot work a couple of months ago in Cambridge to try out both some of the advertisements and also to assess the impact, so I will give you a hint?
We can see about your views towards people with mental health problems, comparing people who saw the advertisements - and these were on poster placards, on sides of buses, on beer mats, in local advertisements in newspapers and radio and so on - versus those who did not see them. People were asked if they would be willing to live with somebody with a mental health problem. Those who had seen the advertisements went from 86 to 95%. Then they were asked if they would be willing to continue a relationship with someone with mental health problems, remembering that quite often getting dropped by your spouse or your partner or your friend is a serious problem, and that went up from 87 to 95%. Next they were asked if they would be willing to live nearby to someone with a mental health problem, and that went up a few percentage points. Then if they would be willing to work with someone with a mental health problem, which went up slightly. So these are the sort of ways we are going to be measuring the impact of this campaign. Just within a couple of weeks in Cambridge, we could see some, modest but still noticeable, improvements in those respects.
Then we asked people, 'Well, what do you think mental illness is? Do you think it is depression?' People who had seen the advertisements agreed with that more; it went up 10 points. 'Is it bipolar disorder?' It went up again - nearly everybody agreed at the end. 'Schizophrenia?' Most people, but after the advertisements, everybody said yes. 'Is it grief?' Split views about that. 'Is it drug addiction?' Not sure. 'Is it stress?' Not sure. So we hope, in the campaign, to also clarify what mental illnesses are and are not, over the next four years.
To summarise, I have talked today about stigma, but more, I have tried to talk about discrimination, namely the behaviours, both by people with mental health problems and towards those people, which are forms of social exclusion. I have given you a summary of some elements of this review, of the whole field of discrimination, and I have gone on to say that there is no reason to be pessimistic, because we now have interventions that we know can work locally, and which can work nationally, from studies already carried out. What we need is the political will and the resources and the investment and the persistence to make this work.
©Professor Graham Thornicroft, Gresham College, 10 December 2008
This event was on Wed, 10 Dec 2008
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham College plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login