24 March 2014
The Work of the Defence Medical Rehabilitation Centre,
Headley Court
Col. John Etherington OBE
My name is John Etherington. I am the Director of Defence Rehabilitation. I am based at Headley Court, and I have worked at Headley Court for many years as a clinical consultant. My specialties are rheumatology and rehabilitation medicine, and I also am involved in sport and exercise medicine.
I have recently taken up a post within the National Health Service, two days a week, working as the National Clinical Director for Rehabilitation & Recovering in the Community for the NHS England, with a view to trying to enhance the rehabilitation services within the NHS.
So, I am going to talk to you about defence rehabilitation and really the take-home messages from that and how it has impacted on the casualties that we have received from Iraq and Afghanistan particularly over the last ten years.
If there is a message about why defence rehabilitation has been successful, it is largely included on this slide. Our rehabilitation services are very much embedded with the acute medical services; there is a very close interaction between what we do in terms of rehabilitation and the surgeons and the other acute teams, but also in primary care where our patients live.
We very strongly believe in this multi or interdisciplinary working. We do not achieve anything except by close team-working.
Although we are in a military environment, if the patient does not want to do something, he will not do it, so focusing on patient-delivered goals is critical: what does the patient want to achieve out of this period of rehabilitation?
Critically, we have a vocational focus. We are paid by the military to get people back to duty. That is our main raison d’etre and therefore the second question we ask a patient when they come and see is, after what their name is, is what is their job – if you do not know what someone’s job is, how can you hope to get them back to work?
We have always been reactive to the service need. In other words, if they are new casualties with this particular type of issue, we have had to respond to it. We cannot say “Sorry, we do not do that.”
Most importantly, I think, and probably the thing that we somewhat lack in the National Health Service is ambition. We want to deliver the very best for these patients and we need to have that same ambition within the NHS.
So, I am the Policy Director for a thing called Defence Medical Rehabilitation Programme, which in fact is separate, and deliberately so, to the defence recovery capability, recovery being the military concept of recovering the patient back into their unit, into the bosom of their regiment, with a view to how do we manage this as an individual soldier, as opposed to the rehabilitation side, which is the medical component. We deliberately keep that separate so that we do not conflict what is best for the soldier. But, essentially, I have got two aims: one is support a thing called Force Generation; and the other is battle casualty and trauma rehabilitation. Why do we do it?
Well, Force Generation is getting a force fit to fight, to deploy, to get it to Afghanistan or to the next hotspot that we are sent to, and you cannot do that if people are not medically fit. So, my job is to get as many people as medically fit as possible to deploy. That is the first bit.
The second bit seems pretty obvious. We should be treating people who have battle casualties or who have had trauma, or the complex medical conditions that we see. But why do we do that? Well, we should be doing it, primarily, because of the humanity issues, but the way I can sell it to the people that hold the purse strings is this is about supporting the moral component of fighting power. What does that mean? Well, it has a real direct effect. If you think that if you go out on that foot patrol tomorrow and loose both your legs, you will be cared for in the best possible way, then you are more likely to go out on that food patrol, and I think we have got good evidence that that works.
So, this has been the nature of the conflicts over the last couple of years. These are pictures predominantly from Afghanistan but equally Iraq.
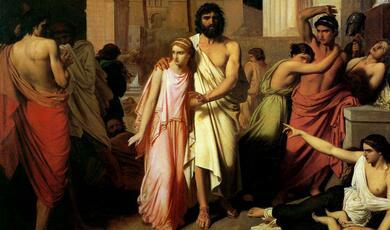
The consequence of war fighting are not new of course, and these are paintings taken from Bell, who was a doctor at Waterloo, and in fact, these sketches, or copies of these sketches are kept at the Royal Army & Medical Corps Museum in Keogh Barracks at well. They are very interesting There is about 20-25 pictures, and all of them are associated with case reports. What we do know is that, of those three, one survived, and that is the chap who is the amputee on the right.
The casualties related to blast and gunshot wound obviously became much more severe and complex, particularly during the First World War, where the first proper approach to rehabilitation, in combination with the plastic and reconstructive surgery that you see here started to occur, and some of the models of care that we use now derive from the First World War, but there was a definite recognition that if you did not address the medical rehabilitative concerns of the patient, not only were you in breach of your guidance in terms of humanity, but you were also storing up problems for the future in terms of those individuals’ care but also discontent. Bear in mind of course, this is at a time when there was a considerable social discontent across Europe.
I think this is quite interesting, that this picture has the title which says “Not downhearted”, and certainly, the picture there is of happy people, in an environment where they’ve been well-supported. Whether that is entirely true is another matter. Certainly the expectations of those individuals, in terms of their recovery from the First World War, is entirely different to the patients that we see today – and more of that in a moment.
In the Second World War – and here is some of Archie McIndoe’s Guinea Pig Club, so burnt patients having some of the earliest forms of pedicle flaps being produced to reconstruct the loss of skin on the face. There was a recognition that, if you want to keep fighting, you need to keep these people fit, and indeed, Headley Court was produced as a result of the War. So, it was not working during the War. There were rehabilitation centres, but it came into being in 1947 as a result of charitable donations, principally for the rehabilitation of these people – Royal Air Force air crew. But over the years, that remit has expanded to all service personnel.
So, the consequences of war today are this. There is a fit paratrooper on operations in Afghanistan, and as a consequence of his stepping on an IED, he is, in this case, he has lost three limbs. Our role is to take him from someone who is incapable of looking after themselves and giving them some limbs, ensuring, as he did, that he got to his medal ceremony, presented with his campaign medal by Prince Charles, within I think about six weeks of him coming to us, and subsequently an independent life.
Here, he is on the Dakar Rally, which he successfully completed.
To do that requires the right sort of substrate to start with, so a determined and focused individual, and the right sort of equipment and the right teams to deliver the outcomes.
We would not have any challenges had it not been for our acute medical services, and I always congratulate them, and indeed thank them, for the incredible job that they have done over the last ten years, and indeed, in terms of innovations, again, military medicine has led, and there is no doubt that the range of injuries are unprecedented, and people would not have survived, even five years ago, with the type of injuries that we have been routinely seeing.
To put that into context, if you look at operational injuries, if you look at the National Health Service compared to the Defence Medical Services, these are the injury severity scores. The average injury severity score within a trauma centre in the NHS is 16-24. In our experience, it is between 36 and 75, 75 being incompatible with life. It is not because people survive and we have had many patients who, in other environments, are incompatible with life. Sir Keith Porter, who is the lead trauma surgeon at Birmingham, who receives the casualties, regularly says that he received casualties from Afghanistan who had been flown 8-9 hours to get into Birmingham, who were fitter and more likely to survive than patients who are knocked down an hour away in Birmingham.
Nevertheless, this is an indication of the challenge of the injuries that we have seen, and certainly, I, for example, have seen a patient who, in Camp Bastion, has received 180 units of blood in one admission, and survived and went on to normal life.
This is an example of the type of patients we have seen, and I give this example as a routine case, not as an extreme example, but a routine case would be a bi-lateral, both legs, above knee amputations, a pelvic fracture, which has been externally fixed here in order to keep it intact, damaged to the bowel, with a subsequent colostomy, and multiple finger and upper limb tendon damage, requiring skin grafting here, and multiple soft tissue loss and skin grafting. That is a packet of his medication that he came to us on. You can see that the wounds have not healed. This is all skin grafted, so the quality of the skin is not very good, and our job is then to get him (a) back on his feet, or someone else’s feet, (b) back to work, and we did. But you can imagine that actually trying to mobilise somebody with no legs is tricky. To mobilise someone with a fractured pelvis and no legs is even trickier, and we have to use different techniques to get them fit again.
Integral to that, and as I said earlier on about multidisciplinary working, are the complex trauma teams. So, we have organised our rehabilitation services in response to the increase in casualty numbers, in teams which are made up of every possible combination of people, be it, in this case, our OT, who is the manager of the complex trauma team and now has over 100 members of staff to manage – doctors, prosthetists , nurses, social workers, physiotherapists, OTs, and our exercise rehabilitation instructor.
So, how do we do it? Well, we set these principles up long before the war started. We sat around in a room and said: what do we think this should be – how do we do it? It has been a very valuable exercise.
You have got to treat people early. You cannot wait three months and say, “Well, we have got a bed for you.” We have to do it next week.
You have got to actively case-manage people. So, with people with multiple injuries like that, you have to, as the rehabilitation consultant, make sure that he is going along that care pathway at the right time, seeing the right people, for the right thing. In the perfect world, it would all happen automatically. You know, those of you who have ever been to an outpatient appointment or awaited an operation will know that it does not always happen perfectly. If, in order to recover that individual, and that process may take three and half, four years, that individual might need 25 operations – who is going to make sure it happens, and who is going to make sure he has rehabilitation at the end of it?
Multidisciplinary working, we have talked about.
Exercise-based rehabilitation is absolutely critical to what we do, and group therapy, which is – that combination is unique to the military, and I will talk about that in a moment.
And also having rapid access to investigations and further specialist advice… So, as you can see, those patients do not come to us a done-deal, fixed, ready for us to rehabilitate. They will almost certainly have to go back for further plastic surgeries, orthopaedic surgery, treatment of infections, other treatments. So, for example, if they have had genital injury, there are issues of fertility, neurological issues to manage, psychological issues to manage, endocrine issues – all of that needs to be coordinated.
We do not just do this in Headley Court, which is in leafy Surrey. We do this all over the world. Headley Court is the specialist centre, the hub of the spokes for defence rehabilitation, and when we talk about early treatment, we do it as early as possible. This is my rehab team, a few years ago actually, in Camp Bastion, and some of those will fly out every now and again to go as far forward as possible, which is safe, to treat our patients with musculoskeletal injuries. Others will be based in Bastion. We have a specific physiotherapy team who look after the critical care support of our patients out in Camp Bastion. So, we have a physio there and an exercise rehabilitation instructor who takes not just British casualties, but all casualties, through their earliest stages of rehabilitation in Afghanistan.
Many of British casualties being severely injured would have come straight back to Birmingham, so they spend very little time in Bastion, maybe 24 hours, before coming back to Birmingham, where, again, we have, embedded within the NHS, set up military rehabilitation teams who start the treatment as soon as that individual’s on ITU, and indeed our consultants visit and talk to the patients and relatives on ITU and start talking to them the day after they have arrived, if we can talk to the patients, or if not, to the relatives, about what the rehabilitation plan is. We are talking about from three years down the line, this is where you will be. That gives people hope and the direction to continue.
So, this early ward-based rehabilitation is critical. It gets people going, gets them out of bed, they do not wait around. We have this weekly ward round with the rehabilitation consultant, who assess the patients and make the plans for them to come to us, advise on surgery and amputation, for example. We do rehabilitation assessment and if we need to stick a prosthetic limb on, particularly upper limb, in Birmingham, we will do it there, and then we plan their rehab pathway.
I would say that we do not just do trauma. In fact, even at the height of the war fighting, over 50% of our activity was related to trauma. Most of the rest of our activity is what the rest of us get on a daily basis. If you are training physically very hard, as an infantryman or a paratrooper or something like that, you will get musculoskeletal injuries, such as a stress fracture of the hip or bad back – this is a prolapsed disc there. So, much of our activity is managing this musculoskeletal and sports and training injuries type things. But the complex trauma has been a feature of what we have done in the last few years, and I am focusing mainly on that, and the neurological rehabilitation, predominantly of those with brain injury.
How do we do it? Well, this is called multidisciplinary bio-psychosocial model, which is a very grand title for using all elements of the team to get people fit again, so we cannot just give you strengthening exercises, we have to think about your mind, and we have to think about what motivates you, we have to think about the social factors. We have to educate you about your illness and how your condition can be rectified, and we have to re-introduce people into a normal lifestyle, and a lot of that is through exercise-based rehab.
Now, we have the advantage in the military in that, actually, although it is not particularly normal in any other context, exercising in a group of people, with your PT kit on and looking slightly stupid, is quite a fundamental part of being in the armed forces. So, turning up for group exercise is quite common in the military and therefore we can use this as a form of work.
How do we do it? We use group therapy. So, we take a group of patients with complex conditions but a broadly similar level of function, we take them through the process, we use a graded programme of exercise – in this case, it is hydrotherapy. Here, we are doing weight training. Bear in mind, at this weight training circuit, many of the patients are amputees, so we make allowances for people’s functions, but we are not saying that because you are an amputee that somehow you are different – you just have less limbs than the rest of us.
And then, out of that programme, we take people off for psychology, physiotherapy, speech and language, prosthetics, nursing, occupational therapy, mental health services. But the core delivery is exercise-based rehabilitation.
Part of the advantage of this group is pragmatic. I can treat a lot of people in a group and give them a lot of treatment as a group, and that is why this model was developed in the First World War. The other part of it is peer support.
Here is an example of one of my early patients treating one of my older patients, and he, as you can say, he is in uniform, showing his prosthetic limb. He worked as a liaison officer between Headley Court and Birmingham. So, having been a patient, he became an expert patient, and he was able to advise these individuals on the practicalities of life. So, this peer support is really important, and really important for the psychological support. We talk about mental health services and psychological support. Do you know, it is much better if that psychological support comes from people who you know and trust, your fellow patients, and I think it makes a huge difference.
So, that means – and this is a timetable, average timetable for a patient – that, on a Monday, Tuesday, Wednesday, Thursday, Friday – Friday, we let them off early because they are usually shattered – these, you have got a full programme, so seven hours a day, five hours face-to-face time of rehabilitation, every day for at least a month. Weekends are free. That intensity is what delivers the outcome, and that is the difference, frankly, I think, between us and the National Health Service. So, you will get 25 hours’ rehabilitation that week, and if you are not, either my staff are not doing their job or you are off skiving. Sometimes, we get some people skiving, but they are usually “retuned” into the programme, put it that way. But the reality is that these individuals are told that you will return, you will go to work at 8.30 and you will finish work at 4.30, and your lunch hour will be at 12, and we do that (a) because it is easier to manage the patients, but (b) because we are trying to get people back into a frame of working. You are not suffering, you are not in a hospital – you are on a course to train to get better, and part of the contract between us is that this is a job of work they are doing. They are still being paid and their outcomes are dependent on how much effort they put in.
We can get patients into Headley or for defence rehabilitation through a variety of ways, either, in this case, the battle casualty might come from Birmingham and then go to Headley Court, or a musculoskeletal injury might go to a primate care rehab facility, primary care physiotherapy, or into what we call our regional rehab units. The point is that they will circle around, depending on their level of function and their needs at the time, and bounce up and down. That has given us a reservoir of rehabilitation treatment.
So, if we had assumed that the only rehabilitation services available to us during the conflict would have been Headley Court, then we would have run out of space very quickly. But it is not, so we can use Birmingham, the patient comes to Headley, they may go on a period of sick leave for rest and to reinforce what they have learnt at Headley Court, then they come back, more sick leave, Headley Court, and they may need to go back to Birmingham for surgery. As they get fitter, what we introduce is the concept of work, so we will try and get them back either to their working environment, if they can, and if they cannot, they might be going through an educational process, through the recovery capability that has been mentioned, back into the regional rehab units or the primary care facility, Headley Court, Birmingham again, cycling around, with the effect of trying to get the right person in the right place at the right time and get them better.
That has been helped because we now have a single electronic patient communication record. So, if I fill in a record on a patient in Headley, it can immediately be seen by a primary care doctor or the regional rehab units, and vice versa.
Vocational rehabilitation has been important to us in terms of preparing people to get back to work, placing them in work, supporting them there, and then following them up. So, from Headley Court, when they are fit enough to go back to work, they will be sent to a work assessment, and if that is successful and they have made sufficient recovery, they will return to their unit. They will have a reduced medical capacity, so they cannot deploy or cannot do certain types of jobs, but then they will be re-introduced to their own work and given a vocational occupational therapist to support them there, who also talks to the employer as well. So, it is all in agreement with the employer, i.e. the company commander or the line manager, to make sure that this individual gets the best chance of work. Now, sometimes that work does not work out. That is as important to us as a successful placement because it shows the individual what they can and cannot do.
Sports, adventure training or other adaptive activities are really important. S, for example, we had at least one of our patients at the Paralympic Games in Sochi recently, and we had six athletes at the 2012 Games. But not everybody wants to be an elite athlete. Some of them want to just play a bit of sport to keep fit or keep active, and we do that, both in a non-adaptive way – so this is amputees and other injuries on a boat, competing against able-bodied people, and they came third in their competition.
Interestingly, one of our physiotherapists introduced the concept of gardening therapy, and I have to say I was a bit sceptical that the average paratrooper would be interested in gardening, but it was very popular, and, as far as I am aware, they did not grow anything untoward. So, in fact, we got a bronze medal, or they got a bronze medal, at the Chelsea Flower Show.
But having these sort of different activities allows people to develop.
So, the big challenge for us has been numbers. This is the years, up into 2013. Blue is Op Herrick, which is Afghanistan. You can see its sudden increase really around 2008/2009. Iraq flattened out. So, basically, a sudden increase in the number of patients coming in to us…
These patients stay with us a long time. If you look at patients in Birmingham, if you look at the total, as the purple colour, you can see that, really, having survived the sort of peak activity really around 2010 and also 2013, the numbers are gradually reducing. If you look at Headley Court, then the numbers have stayed the same, and the reason is because when they leave here, they come to us and they stay with us for up to three years, or longer in some cases.
The big challenge, when I took over complex trauma in 2006, we had four beds and no staff, and 26 patients until the end of the year; the following year, we had ten times the number, and so trying to match the resources against the demand has been our perennial challenge. It is only last year that we have reached a plateau, so new patients coming in have started to tail off.
And what you can see from here is, because of our nature of trying to re-admit people with complex injuries – these are the new cases, in the blue – actually, the thing that drives up the re-admission rate are the re-admission cases coming back.
That is not made any easier if when, in 2009, you suddenly have a new battle. So, that is one battle, and that is the number of casualties occurring as a result of that battle in 2009. It took us until 2013, really, to finish treating the patients arising from that one battle. So, it is very easy to say it is all over, but if we have a big battle in Afghanistan before we depart at the end of this year, that could change.
So, what do we see? Well, this is a femur. This is a thigh bone. This is a gunshot wound through the thigh bone and a fracture there, and you can see the fragments of the round. But he also was burnt and had 70% burns.
This individual was hit by a mortar blast in Iraq, and you can see the right side of his jaw was shattered and he also had a fractured tibia. So, clearly, again, these are complex injuries.
Vehicle blasts were a big problem for us at the time. Here, we have bilateral fractures of the tibia. Here is an example of the nail in the fracture and the non-union of that fracture. Indeed, we learnt a lot of lessons, and one of those lessons is that these fractures do not heal spontaneously. You need to be very aggressive, because the reality is they have got half of Afghanistan still living in there, so these nails have to come out, they have to be debrided, cut the dirt out, they have to be cleaned out, they have to have an external frame put on, and lots of antibiotics. But, interestingly, this individual went back to Afghanistan, admittedly about two and a half years after his original injury. He went to serve back as an officer in Afghanistan.
I think that is probably a quick message to make, is actually, most of our patients want to be there. Most of them want to go back, and most of them, the first thing they say to me is, “When can I go back? When can I get back to my battalion? When can I deploy?” I saw one colour sergeant in the Royal Marines who had lost the best part of three limbs and very seriously injured, and the first thing he said to me, “I love it out there – I want to go back.” So, the concept that somehow we are psychologically breaking people – and I will come onto this in a moment – or that they are not motivated to do this is incorrect. Indeed, I think, in my ten years of treating patients from Iraq and Afghanistan, I can recall of two who did not want to go back. The vast majority are desperate to do their duty. Indeed, in Afghanistan, I remember seeing a young chap who had been shot through the thigh – fortunately, it missed the bone and it was soft tissue wounding, and I said, “It is good news – we do not have to send you back, but you will be about two weeks here recovering in Camp Bastion,” and he burst into tears because he wanted to be back with his mates and he felt he could be back sooner and he felt he was letting them down. After two weeks, he did go back and he served on.
As I said before, drawing it all together is the key, so using this interdisciplinary assessment, specialist input, surgical plans, short and long-term goals, and producing the treatment plan, otherwise, the process does not happen.
Clearly, we have seen a lot of amputees, particularly in Afghanistan, because of the nature of the war fighting there. The difference between these two patients, one of which – that is one of mine, from Iraq, and he is obviously from the American Civil War, is essentially the equipment that we now have. Now, rehabilitation is not essentially about equipment, but in things like prosthetic limbs and wheelchairs, equipment makes a real difference.
These are some slightly old data but, in essence, you know, from the end of 2008/2009, a dramatic increase in the number of double-amputees, the number of single-amputees, and indeed triple-amputees, and that reflects the type of war fighting that we were doing at the time, which was essentially foot patrols and improvised explosive devices, IEDs, mines essentially, going up through the legs as people stood on them. And as they changed the size of the charge within the IED, then you were more likely to lose more limbs.
The problem is, if we say, well, okay, we will just put a prosthetic limb on, the problem is that most of our residual limbs, or stumps, are very similar to this, so they are small. You can see that there has been a heroic attempt at trying to cover the stump with skin, so there is this split skin graft, some flaps, irregularity, and as we use suction as one of the key elements of holding on a prosthetic limb nowadays, you can see that that suction could break down. It is a very short lever, so it is much more difficult to use. That is just a routine case.
In addition to that, if you traumatise muscle and skin and soft tissue enough, then you can induce a thing called heterotopic ossification, and in this case, this is a 3D reconstruction of a CT scan, and this stuff here is basically new bone formation, all formed around within the soft tissues, as dirt, grime, bacteria is all blasted into the soft tissues, and that can clearly be a major challenge in terms of fitting prosthetic limbs and allowing the individual to have some function, and often requires surgery to excise that, which in itself is very challenging.
We have seen a lot of late amputations. A number of our patients have had blast injuries whilst in vehicles, so they have fractures as opposed to losing limbs, and in destroying the joint – there is a big gap here, for example, in the heel bone here, you see that hole there – then what you induce is a low-function, painful limb, and so, actually, what happens is the orthopaedic surgeon’s heroic efforts to preserve the limb leaves with them a painful limb, and they see their mates with no legs running around faster than they are with two legs, so a lot of them go for elective amputation because of this sort of conic pain syndrome.
So, we use prosthetic limbs, and prosthetic limbs have come on a little bit, although, I have to say, having shown this slide recently, you probably would see one or two of these still in the National Health Service – probably not the peg-leg, which we are trying to phase out because it is expensive for the parts, but some of the older ones, you may still use. We do not use them. We use higher functional prosthetic limbs. You could argue why do servicemen get those and the NHS do not? I absolutely agree with you – the NHS should, and the NHS, I will endeavour to make sure, will, but having better prosthetic equipment allows you to have better outcomes, and we are just about to demonstrate that.
It is an intense process. You have got to fit a socket, so that socket is made-to-measure for that individual. Then you have got to put all the fancy equipment on it, and then you have got to teach people how to use it.
You will see people on television using these things, which we call stubbies, and you may wonder why are they not using prosthetic limbs? The reality is that if I give you two new prosthetic limbs, without the muscular control or the balance or the strength, or indeed the physical fitness to use them, you will simply fall over. You have got two hinges there – how do you think you stand up? We give people stubbies to develop the core stability, the physical strength and the endurance, and not least the strength of the stumps to withstand the pressure going through them. So, it is a process, and a lot of the lads will go away with very fancy lower limb prostheses, but may end up, in the house, using stubbies because you can slip them on in two minutes, if that, and pootle around, go to the shower, make a cup of tea, etc. etc. But when they are working or going out, they will put their prosthetic limbs on.
What has really transformed our management of those, with above-knee amputations, are these new microprocessor knee systems. So, this is a thing called a Genium. This is now the standard piece of equipment that we use. It has a microprocessor in it. It measures, at least 50 times a second, where the knee is in time and space, where the forces are going up through that, that limb, what the angle of rotation is around the knee joint. And, if you imagine your leg, what you want of a leg in this position is to be immensely stable, and it is. What you want to do when it is walking is to be unstable, so I want to be able to bend that knee, and now it is unstable. I can do that, you can do that, by muscular control, fed into by the nervous system. You do not have any muscular control or a nervous system into a prosthetic limb. So, you have to be able to either balance it, in the old days, which is a bit of a challenge, or in Douglas Bader type style, you lock the knee so you walk with a stiff knee, or you use a microprocessor, which basically, depending on the stage of your gait, can tell where you are and can tell even if you are putting your foot down to walk down the stair, so it will give you give to allow you to put the next foot down, and that will give but will not collapse. They are great. That one costs £27,000, just that, and clearly, we give out a lot of pairs.
That was the original one. That is the c-leg. That was £16,0000. The Genium is £27,000. The X3, which is the American version and is effectively waterproof, costs £42,000, although we have managed to beat them down on the costs for that. But they are expensive, but they are effective.
This is also the next generation of prosthetic limbs. So this is a powered ankle. All of those are passive – you use muscular strength to move that limb across. These use power – it is the motor in that ankle which will drive the plant inflection of the foot and tow you off. Are they any good? Well, we have got one of our prosthetists who is actually an amputee, and funnily enough, he seems to have that on trial quite a lot. They are very good. They seem to be very good and much more reliable than the original. This is still pretty much early stage, almost a prototype, but they are expensive. They are particularly good, if you imagine, for someone who has had a hindquarter amputation, so has taken off the entire hip, so have no hip joint – how do you fit a prosthetic limb on that? Well, you effectively sit on the prosthetic limb. If you have got power, then you can drive that person forward in these very complex injuries.
Do they work? Yes, they do actually. We got a lot of pressure to stop prescribing them because we were told they did not work, but they reduce the energy expenditure when walking at higher velocities, therefore people walk more, so their overall energy expenditure goes up, which is probably good for their health, and better quality of life measures.
The data, because of course we are now coming to sort of the point where we can analyse our cohorts, would suggest that these patients are getting enhanced function, reduced pain, particularly back pain.
Their six-minute walk test for our bilateral above-knee amputees is now approaching that which we would expect in this room, so our bilateral amputees can walk as far in six minutes as you can. That is unheard of. Most bilateral amputees in the world, and probably in this country, will not walk regularly. Most of ours do – the vast majority will.
And vocational outcome, well, things have changed. Since the recovery capability came on-board, we have now got a better outlet for our patients who are triple-amputees, who actually probably just need good support and education, preparing them for the outside world. But, in the early days, we were sending them back to work as part of that programme of getting them back. You may be surprised to hear that, from point of wounding, the average time to getting someone back to work, an amputee back to work, in the military, is seven months, so that includes their wounding, hospitalisation, and their first stage rehabilitation.
What about their overall outcomes? Again, this is on our amputee population. This is slightly older data. There is a thing called the SF-36, which measures a variety of components. There is an overall physical components scale. What we saw was there was a significant improvement between admission and six months later, in terms of physical component. It has not reached the normal population, but it is higher than original.
Interestingly, when we looked at the mental components summary, we were initially disappointed to say that there was not a change in the score during the period of rehabilitation, and then when we looked at the data, we realised that is because the mental health was above normal at the start of presentation, when they first came to us. Now, admittedly, that normal was taken from the American population – I am not sure what that says, but nevertheless, it does reinforce one of our findings, is that many of our patients when they present to us will have what we would call an adjustment reaction, maybe anxious, maybe angry, maybe distressed. If you are 22 and you have lost both legs, what is your immediate reaction going to be? They may be suffering from nightmares. They may have difficulties in concentration. They may also be under lots of medication for pain and things like that. What we have found is, most people, those adjustment reactions recover quite quickly, and the peer support is critical to that. What we have spent a lot of time doing is saying, if you are feeling hacked off because you have lost both your legs, then that is normal. If you are having the odd nightmare, that is normal – you will it will get better. And talking to the other guys helped them – not everybody, but helped them. Even our very complex patient group, only about 10% have significant mental health problems, such as depression or PTSD. I think part of that is this peer support and the fact that we are watching their every move, if you wish. But it is slightly counter to what the general view is of the mental response to these sort of injuries. Now, clearly, we do not know what it is going to be like in twenty years from now, but the initial stage was very encouraging.
Traumatic brain injury is something we see a lot of. Interestingly, it did not increase dramatically during the war, except later on, about 2009/2010. So, in this case, this is a traumatic brain injury with high signal in the occipital region. This is the result of a gunshot wound. So, there you can see the track of the round coming in through here and out through here, and the skull has been removed, partly by the round and partly by the surgeon to relieve the pressure. Now, that individual survived and is living independently, and I would say the reason for that is the outcome of the rehabilitation that they received. So, we have just recently looked at a group of neurologically injured patients, about 101 of them, and at four months after discharge, 85% are living independently. After severe brain injury, most of them will go back to independent living.
If you look at employment status, 77% are either in employment or employable and in the process of going through job hunting. Again, that is unprecedented in terms of outcomes. It is early days. Again, it is only four months post-discharge, but it does show that, with the right intensity of treatment, that you can get people independently living and working.
This is peripheral nerve injury. This is interesting because the classic finding with all military medicine is we make great discoveries and headway and then we forget all about it. This is particularly true in peripheral nerve injuries. In this case, a helicopter load-master in a crash, severe burns and damage to the peripheral nerve injuries. If you reconstruct those peripheral nerves in the right way, if you have the right aggressive approach to managing them, they recover very well. So, at presentation, more people had poor outcomes than good as a result of their peripheral nerve injuries. If you operate on them, you can transform it the other way around, so you can actually change the balance. The trouble in medicine, in peripheral nerve injury management, is it is very neolistic – it is very, well, it is going to get better, it is going to get better – if it is not, we will just ignore it and nothing you can do about it. We have demonstrated, once again – I say “once again” because it was demonstrated by Robert Jones in the First World War – that you need to actively manage these cases.
So, another innovation – this, we have just tried – is a thing called osseo-integration. Now, the problem, as you have seen, in fitting these prosthetic limbs, is often getting the right socket. If you do not need the socket, then you make life a lot easier. This is the second innovation. In fact, this surgeon is from Australia, and what he is done is to put a metal post into the femurs of this individual patient, and then you can simply clip your prosthetic limbs to the metal posts and then start the rehab, a bit like a dental post. As you can imagine, there are issues of infection and other issues, and so this is a first attempt, but you can imagine trying to fit a socket onto that limb is very difficult.
Another innovation we have tried, we had a chap who lost his arm, very high, from a grenade attack, had a lot of post-trauma peripheral nerve pain, phantom pain, essentially. We, in collaboration, with an Austrian surgeon, we re-aligned the nerves, the brachial plexus of his shoulder, implanted them in the residual muscles of his chest, re-educated those muscles to do different jobs, attached mio-electric sensors over the muscles, and then, by simply thinking about flexing his elbow, he can flex a prosthetic limb elbow or rotate the hand out or produce a grip. Interestingly, since we have done this, all his pain has gone as well. So, this sort of bionic limb, with this integration into the muscles of the residual…well, not even quarter in this case, is a new innovation, is being done really only in Chicago. The surgery is in Vienna, but we are doing the rehabilitation and prosthetic manufacture for him, and been a great success.
So, what happens if you are in the NHS and you fall off your roof and you are a taxpayer, at the start, and you have got two children, and you are self-employed, what happens then? Who rehabilitates them?
This chap, Ludwig Guttmann – you may have seen a recent film about “The Best of Men” – set up spinal injuries rehabilitation in Stoke Mandeville during the Second World War, and was the founder, effectively, of the paralympic movement. But his axiom, which I have to confess I had stolen, not knowing it was his axiom – I thought it was my axiom and crikey, I am clever – is we should be producing taxpayers. Why is that individual being looked upon as somebody who cannot contribute for the rest of his life? My soldiers do not – they just want to get on, get to work, get a fast car, find a girl, and get on with their life. That is it.
These are some of the guys that have. Winter Olympics, this chap won, I always forget, three silvers…very gutted that he did not get the gold, but highly successful and driven individuals.
So, just to close, this is a picture from the First World War of similar sorts of patients, similar sorts of injuries, slightly old-fashioned wheelchairs, and hopefully a slightly different outcome.
Thank you very much.
© Colonel John Etherington OBE, 2014


 Login
Login