Hygeia and Panacea: Is prevention better than cure?
Share
- Details
- Text
- Audio
- Downloads
- Extra Reading
Better sanitation and hygiene, coupled with immunization, have dramatically reduced illness caused by exposure to microbes. For those who do fall ill, a galaxy of drugs and medical procedures have been invented to treat conditions of all kinds. Among all these means of prevention and cure, which have made the biggest impact on human health?
Download Text
Hygeia and Panacea: is prevention better than cure?
Christopher Dye (dyec@who.int)
What's the single best method of prevention or cure ever devised to improve public or personal health? a As you mentally sift through possible answers, consider the old adage that prevention is better than cure. It has a nice ring, but is it really true.
Where does that proverb come from, and what is meant by it? Is it an old wives' tale, a dangerous folk myth, or a naturist's plug for wholesome lifestyles? In the words of American humorist Jack Handey, “Dad always thought laughter was the best medicine, which I guess is why several of us died of tuberculosis.”
Or perhaps it's a self-evident and universal truth based on economic wisdom? There are some classic examples of cheap and simple ways to prevent nasty diseases. Celebrated in the annals of preventive medicine is the discovery made in the mid 18th century by James Lind, a British naval officer. Lind found that lime juice prevents scurvy (among "limeys"). He published his "Treatise on the Scurvy" in 1754, though carrying lime juice on ships was made mandatory only 50 years later.
Scurvy is a nasty disease, and fatal if left untreated. Symptoms include corkscrew hair; ruptured blood vessels; skin become dough-like; gums redden, recede and blacken until teeth become loose and fall out. There are skeletal defects, including bowed legs, stunted bone growth, and swollen joints. Blotches appear all over the body and any bruise or exertion can result in internal bleeding.
Lime juice contains ascorbic acid or vitamin C, which is important in the formation of collagen, and any deficiency interferes with normal tissue growth. Vitamins were not discovered until 1912 (and vitamin C not until 1928), but Lind didn't need to know that this was the effect of a vitamin. He made his discovery, remarkably, using an early prototype of the controlled clinical trial.
Erasmus. The idea that prevention is better than cure is much older than Lind, and the saying can be traced back to the 13th century. However, it's reasonable to suppose that Erasmus played a role in propagating the expression, which was included among his collected Adagia. Erasmus – known for his cultivation of common sense as applied to human affairs – wrote a series of books with appealing titles. "On Civility Among Children" certainly has resonance among the parents of teenagers.
I am going to explore the prevention-cure dichotomy more formally. But first, here is a reminder of what our preventive and curative methods need to overcome. I've described more fully in previous lectures – the distribution of the 60m deaths each year, 10m among children. For communicable (infectious) diseases, the death rate is far higher in low- and middle-income countries than in rich countries. For chronic diseases, the death rate is higher in rich countries. But poor countries also have a higher mortality rate from chronic than from infectious diseases.
Part 1. When prevention is better than cure
To discuss some more formal analysis, we need to consider how health, or conversely illness, is measured. One problem is how to put illness and death in the same currency? Another is how to compare different kinds of medical conditions. How, for example, do you compare rabies with heart attack?
A standard index or metric is called the Disability-Adjusted Life Year (DALY), effectively a year of healthy life lost, where DALY = years lost to (illness × disability weight) + years lost by death.
There are numerous points of controversy surrounding the use of DALYs. One of them is that each type of disability is given a score between 0 (perfect health) and 1 (death), around which there is some (approximate) consensus in the medical profession. There are some examples in this slide.
Armed with this means of analysis, we can begin to investigate how best to spend money to improve public health, i.e. we can do cost-effectiveness analysis. I stress "public health" here because this is the way governments look at the problem. You and I as individuals think differently about prevention and cure, and I'll come to that later. The fundamental difference is that governments want to protect the largest number of people, given available resources. Put crudely, they don't care who is protected, just how many. Whereas you and I care most about ourselves, and our friends and families.
In the case of lung cancer, in cost-effectiveness analysis done from the perspective of public health, an ounce of prevention is definitely worth a pound of cure. Lung cancer is essentially incurable. Of the order of $100,000 of palliative care will buy you a year of "healthy" life (an average for various terminal cancers). By contrast, preventive measures such as taxation, nicotine replacement therapy, and no-smoking campaigns are much cheaper, costing $1000 – 10,000 per year of healthy life.
Tobacco tax really works. These data from New Zealand are typical. As an aside, you may not know that the word "immunity", meaning insensitivity to disease, comes from the Latin noun "immunitas", which means exemption from taxation. Here it's the taxation that prevents disease.
You might already be asking whether this kind of analysis really captures all that governments (for example) need to know to make the right decisions about investing in health. Here is a thought experiment. Would you, as a health minister, choose prevention of palliative care for terminal cancer, if it cost the same for each day of healthy life?
Cost-effectiveness analysis is a tool for making choices between, say, options for managing an epidemic of cancer. Spending is expressed in terms of real money; outcomes are expressed as improvements to health (e.g. DALYs). Another way to do the economics is to ask whether health benefits, also expressed in monetary terms, are worth more than the money we need to invest. Putting health in monetary terms is always controversial, but that is essentially the approach taken in the recent Stern Review on climate change. The bottom line is "The benefits of strong, early action on climate change outweigh the costs".
This is a reconstruction of Michael Mann's "hockey stick", first published in 1998. It shows the temperature changes over the past 1100 years, and the recent rises that must be stopped. Smoothed reconstructions of large-scale (Northern Hemisphere mean or global mean) surface temperature variations from six different research teams are shown along with the instrumental record of global mean surface temperature. Each curve portrays a somewhat different history of temperature variations, and is subject to a different set of uncertainties that generally increase going backwards in time. This set of reconstructions conveys a qualitatively consistent picture of temperature changes over the last 1100 years, and especially the last 400 years. The evidence allows us to say now, with a high level of confidence, that global mean surface temperature was higher during the last few decades of the 20th century than during any comparable period during the preceding four centuries.
These are some of the possible health consequences of a continuing rise in temperature. At lower temperature rises (1-3°C) , it is possible to speculate on specific conditions such as malaria, malnutrition, diarrhoeal disease and so on. The impact of higher temperature rises (5+°C) is very much harder to forecast, especially the many indirect consequences of widespread disruption caused by large-scale population movements.
The goal is to stabilize CO2 emissions. Stabilizing at or below 550ppm CO2e would require global emissions to peak in the next 10-20 years, and then fall at a rate of at least 1 - 3% per year. By 2050, global emissions would need to be around 25% below current levels. These cuts will have to be made in the context of a world economy in 2050 that may be 3-4 times larger than today - so emissions per unit of economic productivity (measured as GDP) would need to be just one quarter of current levels by 2050. The later we leave it, the harder it will be to stabilize CO2e. Weak action in the next 10-20 years would put stabilization even at 550ppm CO2e beyond reach.
Here are the summary results of cost-benefit analysis, in which some frankly heroic assumptions are now tolerated by a growing consensus that human CO2 emissions really are pushing temperatures upwards. Estimates of resource costs suggest that we need to invest around 1% of GDP (upper bound) to reduce CO2 emissions so as to achieve stabilization at 550ppm CO2e. The excess of benefits over costs (net present value) from implementing strong mitigation policies this year would be about $2.5 trillion. These are the benefits that could flow from actions taken this year; many of the costs and benefits would be in the medium to long term. An important corollary is that there is a high price to delay. Delay in taking action on climate change would make it necessary to accept both more climate change and, eventually, higher mitigation costs. With 2-3°C warming, the cost of climate change could be equivalent to a permanent loss of around 0-3% in global world economic output, compared with what could have been achieved in a world without climate change. With 5-6°C warming, models that include the risk of abrupt and large-scale climate change estimate an average 5-10% loss in global. GDP, with poor countries suffering costs in excess of 10% of GDP.
Gordon Brown also believes in investment for prevention, through his International Finance Facility for vaccines and sanitation. “The rates of return from upfront investment in water and sanitation would significantly outweigh the costs of borrowing from bond markets…” (Human Development Report 2006).
Smallpox. The value of disease eradication is harder to capture in economic terms because short-term investment brings rewards for eternity. This series of photographs illustrates the evolution of skin lesions in an unvaccinated infant with the classic form of variola major. (a) The 3rd day of rash shows synchronous eruption of skin lesions; some are becoming vesiculated. (b) On the 5th day of rash, almost all papules are vesicular or pustular. (c) On the 7th day of rash, many lesions are umbilicated (with central pits), and all lesions are in the same general stage of development. Retrospectively, would anyone deny that smallpox eradication was worth the effort?
Three key figures in smallpox control, from inoculation to vaccination to eradication. (a) In 1718, Lady Mary Wortley Montague reported that the Turks have a habit of deliberately inoculating themselves with fluid taken from mild cases of smallpox. Lady Montague inoculated her own children in this manner. (b) In 1796, an English country doctor, Edward Jenner, observed that milkmaids would sometimes become infected with cowpox through their interactions with dairy cows' udders. Cowpox is a mild relative of the deadly smallpox virus. Building on the foundational practice of inoculation, Jenner took infectious fluid from the hand of milkmaid Sarah Nelmes. He inserted this fluid, by scratching or injection, into the arm of a healthy local eight year old boy, James Phipps. Phipps then developed symptoms of cowpox infection. Forty-eight days later, after Phipps had fully recovered from cowpox, Jenner injected some smallpox-infected matter into Phipps, but Phipps did not later show signs of smallpox infection. He was apparently immune. (c) Donald Henderson led WHO's eradication campaign until its work was completed in 1977.
These smallpox inoculation devices illustrate both the simplicity of the idea and the complexity of the task. Left to right, from upper left corner: three examples of scab protectors (used after inoculation; early 20th century); two types of current disposable devices; bifurcated needles (a significant invention in 1968 because they used less vaccine and could be sterilized and reused); ivory vaccination points in glass carrier with wood shell (1900); vaccinator with metal carrying tube (19th century); spring lancet (1930s); glass and ivory points; round cowpox scab carrier (1860s, to transport vaccinating material); folding vaccinator (early 19th century); trigger vaccinator (1866); ivory-handled lancets with box (18th century); and drum vaccinator (19th century). The photo shows a man with the distinctive smallpox blisters that often left permanent scars.
One view is: never mind the economics, "Just eradicate the disease and let the sceptics talk to each other" (UNICEF). However, while the cause may be noble, the coffers are never bottomless, and political support is never unwavering for a costly enterprise that does not come with an absolute guarantee. In the case of smallpox, the external cost of $125 million was a trivial price for one of the great public health successes of all time.
Through the success of the global eradication campaign, smallpox was finally pushed back to the horn of Africa and then to a single last natural case, which occurred in Somalia in 1977. A fatal laboratory-acquired case occurred in the United Kingdom in 1978. The global eradication of smallpox was certified, based on intense verification activities in countries, by a commission of eminent scientists in December 1979 and subsequently endorsed by the World Health Assembly in 1980.
The next disease to be eradicated must be poliomyelitis. Polio is caused by a highly infectious virus, which invades the nervous system and can cause total paralysis in a matter of hours. The virus enters the body through the mouth and multiplies in the intestine. Initial symptoms are fever, fatigue, headache, vomiting, stiffness in the neck and pain in the limbs. One in 200 infections leads to irreversible paralysis (usually in the legs). Among those paralysed, 5–10% die as breathing muscles become immobilized. I can show you a picture (left) of young Indian boy crippled with polio, and then I can tell you that there is an excellent vaccine that could have prevented this (right). You will think it tragic, or even scandalous, that kids all over the world have not been protected against polio – that this simple preventive measure is not available everywhere, or that polio has not yet been eradicated.
This is the March 29, 1954, cover of Time magazine, featuring Jonas Salk. Polio vaccines were developed in the 1950s, chiefly by Jonas Salk and Albert Sabin. The main advantage of Salk’s killed virus vaccine was safety - killed virus cannot cause disease. Its main disadvantage was that the formaldehyde used in its manufacture caused the immune system to recognize killed virus differently from live virus, possibly risking a shortened period of immunity. It also had to be injected. Results of trials with small numbers of children in 1952 encouraged the adoption of Salk’s vaccine for a large-scale trial in 1954. Meanwhile, Albert Sabin continued developing his live-virus vaccine. Like others, Sabin strongly disagreed with Salk’s approach of using injected “killed” virus. He believed that long-term immunity could only be achieved with a live, attenuated—or weakened—virus. An important feature of Sabin’s oral polio vaccine (OPV) was that immediately after vaccination, people shed weakened virus in their faeces. This boosted immunity for others in the community and gradually reduced the number of people susceptible to polio. Between 1963 and 1999, Sabin live vaccine largely replaced Salk killed vaccine everywhere in the world. However, because the live virus in the vaccine occasionally became strong enough to cause actual disease, Salk killed-type vaccine has replaced the live type in the United States.
In 1988, WHO's World Health Assembly adopted a resolution for the worldwide eradication of polio. The campaign was based on high infant immunization coverage, with four doses of OPV in the first year of life. Polio cases have decreased by over 99% since 1988, from an estimated more than 350 000 cases in more than 125 endemic countries, to 1951 reported cases in 2005. In 1994, polio was declared eradicated in all of the Americas. In 2006, only four countries in the world remain endemic for the disease - the lowest number in history. However, some major obstacles to eradication remain, notably in India, including high transmission where there is poor sanitation, high population density, inadequate vaccine coverage and low vaccine efficacy.
Part 2. When cure is better than prevention.
If the etiology or cause of disease is unknown then prevention is unlikely. Leprosy is caused by a bacillus, Mycobacterium leprae (a distant relative of the TB bacillus).Remarkably, we still don't know for sure how it is transmitted, but it is probably spread by airborne droplet infection. The first outward sign of leprosy is loss of feeling in a patch on the skin. Leprosy causes disability and even blindness if untreated by attacking nerves under the skin, leading to loss of feeling, paralysis and unfelt injury of the hands, feet and face. It is difficult to catch, and probably cannot be caught by physical contact (e.g. by handshake). Over 95% of people are naturally immune to the disease. It is curable with Multidrug Therapy (MDT), and after only a few days on treatment, sufferers are no longer infectious. Surrounded still by myths, stigma and fear, it is more than a medical condition without an effective vaccine, which is why early detection and treatment with MDT are so vital. Leprosy remains a public health problem in 24 countries, and India, Brazil, Indonesia and Myanmar have the highest numbers of cases. over three quarters of a million new cases are detected each year - over 2000 people every day.
Malaria causes over a million deaths each year, again mainly among young children. The curative method here is the most cost-effective – rapid case management of young children with high fever. As in the case of palliative care for terminal cancer, many people might attach greater value to prevention than is suggested by cost-effectiveness analysis.
Part 3. When cure is also prevention.
The cure of infectious diseases, such as tuberculosis, also reduces transmission. Curing active TB cases with drugs is the most cost effective way to recover years of healthy life, but cure is also prevention. TB can also be prevented by treating – with a cheap and safe drug called isoniazid – people who are infected, but who do not yet have active disease.
The problem with this strategy is that 90% of the people who are infected – i.e. positive on a Mantoux test – will never develop active disease. So there is little incentive for them to take drugs daily for at least 6 minths.
Part 4. When cure is the sister of prevention.
As is implied by Greek mythology. "I swear by Asklepios, Hygeia, and Panacea, and I take to witness all the gods…" So runs the opening part of The Hippocratic Oath. Asklepios represents healing in the medical arts, while his daughters Hygieia, Meditrine, and Panacea ("all-healing") symbolize the forces of cleanliness, medicine and healing, respectively.
Diarrhoeal diseases are responsible for nearly 2 million deaths each year, mostly among children. There is a wide range of preventive and curative methods, with very variable costs for every year of healthy life gained. The principal curative method for children, oral rehydration therapy, is much cheaper, for example, than large-scale sanitation projects, but more costly than small-scale protective methods such as water pumps and pit latrines.
These are the 60 countries in the world where most children die, the majority of course in Africa and Asia.
There has been variable success in reducing child deaths around the world. The rate of decline in Africa has been especially slow, but no region has achieved the target set by the UN, which is an average annual reduction of more than 4% per year.
Most of these preventive and curative interventions are cheap. To reach UN targets – and the targets countries should setting for themselves – the obvious conclusion is that they should all be used together.
Part 5. How individuals approach prevention and cure.
We as individuals make decisions in a different way from governments. If we have the choice of prevention now rather than cure later, why would we ever take the risk? There are at least 6 reasons, as laid out here.
We can think of the value of prevention – how risk averse you are – in terms of insurance. How much would you pay to ensure that you do not suffer? Here are some points of comparison. Roulette's expected value is about -5% of the amount bet. Insurance is worse than roulette, though it is different. In roulette, you take on the risk by playing. In insurance, you pay the company to assume a risk for you. For the best health insurance plans, the expected value of an insurance policy is about -10%, relative to the amount bet, the insurance premium paid. Some insurers sell policies to individuals or small groups with medical loss ratios of 60% or less. These policies' expected value is -40% of the amount bet, or worse. But it's more complex than that – some people will get insured only for unaffordable costs (major illness); some cannot afford even the basic premiums.
For much more on risk, see the lecture by my predecessor, Keith Kendrick, "Why do we gamble and take needless risks?" (www.gresham.ac.uk). Michael Mainelli will also ask, in a lecture to be given next March, "Does society risk my life through safety?" My point here is merely that the decisions we make as single individuals are different from the decisions we make on behalf of whole populations. The latter should take account of the former.
Part 6. Magic bullets and Nobel prizes.
Is cure cleverer than prevention? Though most Nobel Prizes are for basic science, those for cures and therapies outnumber those for prevention by a factor of 6 to 1.
The term "magic bullet" was first used in this sense by the German scientist Paul Ehrlich to describe antibody and, later, the drug salvarsan that he created to treat syphilis. Salvarsan, based on arsenic, turned out to have deleterious side effects; however, the phrase "magic bullet" has become associated with Ehrlich, Salvarsan, and by extension any highly desirable drug.
Penicillin. The roots of penicillin's reputation as a miracle drug were planted in 1942, when it pulled Anne Miller, a 33-year-old patient in a hospital in Connecticut back from the brink of death. She had a streptococcal infection that nearly killed her following a miscarriage. Her doctor had another patient, John F. Fulton, who was a medical professor at Yale and, more important in this situation, a friend of Howard Florey, an Australian pathologist at the University of Oxford who was spearheading the development of penicillin as a drug. Fulton was able to pull strings to have 5.5 g of penicillin sent from the pharmaceutical company Merck in New Jersey, which was helping produce the drug. Within 24 hours of first receiving penicillin, Miller was on her way to recovery. She died in 1999, aged 90.
The antibiotic properties of penicillin were first noticed in 1928 by Alexander Fleming, a microbiologist at St. Mary's Hospital in London, when he saw nothing but dead bacteria surrounding the mold, later identified asPenicillium notatum, that contaminated a culture of staphylococcus bacteria. In later tests, Fleming found that the secretion from the mold was active against a number of bacteria, but he also found that penicillin – its composition then unknown – was unstable and its antibacterial activity short-lived. (Most of the penicillin administered is rapidly cleared from the body by the kidneys. In the early days, researchers would reuse penicillin extracted from urine.) Fleming stopped working on penicillin in 1935, but his 1929 paper came to the notice of Ernst Chain, a biochemist working with Florey, in 1938. Chain suggested to Florey that they undertake research on penicillin, but they did not start until 1939. When penicillin was being developed during World War II, the British researchers rubbed penicillin spores into their clothing in case they had to destroy their research to keep it from the Germans.
Aspirin. Hippocrates, wrote about a bitter powder extracted from willow bark that could ease aches and pains and reduce fevers as long ago as the fifth century B.C. The ingredient of willow bark that is both bitter and good for fever and pain is a chemical known as salicin. Leroux showed in 1829 that salicin is this active willow ingredient. For many years it, salicin, salicylic acid and close relatives were used at high doses to treat pain and swelling in diseases like arthritis and to treat fever in illnesses like influenza. Felix Hoffmann of Bayer & Co wanted to find a chemical that wouldn't be so hard on the stomach lining (his dad's). He found that acetylsalicylic acid (ASA) could not only could reduce fever and relieve pain and swelling, but he believed it was better for the stomach and worked even better than salicylic acid. Aspirin is often used as an analgesic (against minor pains and aches), antipyretic (against fever), and anti-inflammatory. It has also an antiplatelet (“blood-thinning”) effect and is used in long-term low-doses to prevent heart attacks and cancer. Low-dose long-term aspirin irreversibly blocks the formation of thromboxane A2 in platelets, producing an inhibitory effect on platelet aggregation, and this blood-thinning property makes it useful for reducing the incidence of heart attacks.
British pharmacologist Sir John Vane (1927-2004) shared the 1982 Nobel Prize for Physiology or Medicine for his work on prostaglandins and related biologically active substances. His work on aspirin showed that it inhibited the synthesis of prostaglandin.
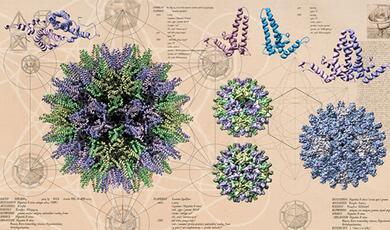
I'll tell you about just one other wonder-drug, praziquantel (PZQ). If you've heard of it, then you're likely to be either a British vet or a tropical parasitologist. 250 million people are infected with schistosomes, and PZQ kills adults worms in a single dose. The picture shows an entwined pair of male and female schistosomes. Adult pairs live in the small veins of human hosts, where the female produces about 3500 eggs per day. Of the trematodes, schistosomes are unusual in that the adult stages have two sexes (dioecious) and are located in blood vessels of the definitive host. Most other trematodes are hermaphrodite and are found in the intestinal tract, or in main organs such as the liver.
The lifecycle of schistosomes includes two hosts: a definitive host (i.e. man) where the parasite undergoes sexual reproduction, and a single intermediate snail host where there are a number of asexual reproductive stages. People get infected when they spend time in water. Kids are measured up for treatment with the tablet pole, which ensures the right dose for a given height.
In summary, is prevention better than cure? In formal analysis, not necessarily: First, quite trivially, the aetiology of some diseases is unknown, so they cannot be prevented. Second, prevention versus cure is not always the right question. Often both are needed and feasible, for example to reduce child mortality in less developed countries. Third, we value more than is captured in formal analysis, which should be thought of as giving guidance, not setting rules.
WHO straw poll. For a group of people who spend most of their time thinking about how to get drugs to TB patients, they turn out to be ardent preventionists. What do you think: is prevention better than cure?
Source material provided on request.
© Professor Christopher Dye, Gresham College, 23 November 2006
This event was on Thu, 23 Nov 2006
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham College plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login