Lungs, Gut, and Skin: Biological Interfaces with the Outside World
Share
- Details
- Text
- Audio
- Downloads
- Extra Reading
We interface with our environment via the air we breathe, the food and water we eat and drink, and through physical contact via our skin.
This lecture explores how these biological barriers act to protect us against toxins and toxicants, through an exploration of dose, detoxification and elimination mechanisms, antioxidant defences and innate immune mechanisms.
Download Text
Lungs, Gut, and Skin: Biological Interfaces with the Outside World
Professor Ian Mudway
27th March 2023
This is the third of my lectures examining the impact of the environment on health. In the first I introduced the exposome concept, to link the impact of life long exposures to environmental stressors to adverse health effects, before considering the impact of air pollution on lung and cardiovascular health. Here I want to bring these two topics together by focusing on how we interface with our environment and have evolved to live within our complex chemical environment.
It would appear if you read our news coverage that we have quite a lot to be concerned about, microplastics in the body, an endless series of studies demonstrating the adverse impacts of air pollution (for which I’m partly to blame), per- and polyfluorinated alkyl forever chemicals, acrylamide in burnt toast and roast potatoes, hazardous household chemicals everywhere, e-cigarettes, pesticides, the list seemingly goes on and on. Indeed, you could argue, as I did in my first lecture, that the chemical landscape isn’t getting any easier, with the number of unregistered chemicals and chemical derivatives easily outstripping our capacity to evaluate their toxicity through conventional approaches. You could even be forgiven for thinking that we’re an endangered species, slowly poisoning ourselves in a chemical haze, yet we prevail. We prevail because we are not without defences, not least our biological barriers, our skin and mucosal barriers.
An average human, if there is such a thing, has an estimated skin surface area of around 2 m2, the area of the gastrointestinal tract varies massively within the literature, but has been estimated at around 30m2, whilst the lungs have a mucosal surface area of somewhere between 50-130 m2. The values vary widely, reflecting how they were derived, based on autopsy, informed by histological investigations of tissue biopsies. For example, the skin values assume a smooth manikin like surface, but if you incorporate the various invaginations related to hair follicles and sweat glands the figure increases toward 25m2. Overall, therefore we can assume that about 200 m2 of us directly interfaces with our external environment, either via the 22,000 breaths of air we breathe each day, the food we consume, or via physical contact.
So take home message number one, there’s a great deal of us in contact with a great variety of potential toxins and toxicants in our environment. Should we be concerned?
This really requires us to focus on some core principles of toxicology and how we measure hazard to inform risk. This is something as humans we are instinctively not very good at. Take for example to extreme scenarios, both clear hazards in their own way. Pianos, one might argue, are not particularly hazardous, but should one fall from a great height onto an unexpecting individual the hazard and risk are both high, but unlikely to transmit to wider population risk . In the second example, eating fast, processed food, is not inherently hazardous, but a poor diet over a long period of time will confer an increased risk of poor cardiovascular health, and because lots of people eat unhealthily the impacts, the overall risks, will be greater. So essentially the risk reflects both the hazard or toxicity, but framed within the context of the likely exposure. The dose determines whether something is a poison, but other factors are also at play.
Toxicity may be modified by gender, age and individual genetic variations which impact on how chemicals entering the body are metabolised, or how protective adaptations are mounted at the cellular and tissue level. But the other factor that is highly pertinent regarding environmental toxicology is the number of individuals potentially affected. For example, an occupational exposure to highly toxic agent is likely restricted to workers, or individuals living with workers (such was the case with asbestos), whilst low toxicity agents in common food stuffs, or in air are likely to reach a larger exposure group and therefore have a larger aggregate effect, even if they have a relatively low intrinsic hazard.
Clearly the first determinant of the potential toxicity of a toxin, or toxicant is how much is absorbed into the body through the skin, lung or gut mucosa. Thereafter, whether there is local metabolism, or distribution to other organs for metabolism, such as within the liver. Whilst the metabolism of foreign materials, xenobiotic metabolism, aims to reduce the toxicity of the of the absorbed compounds and convert them into a form, or metabolite that can more easily be eliminated, in certain cases more toxic metabolites may be formed, that can result in overt toxicity at the tissue level. For example methanol is converted in the liver to formic acid via formaldehyde, which inhibits mitochondrial cytochrome c oxidase, causing hypoxia at the cellular level, and metabolic acidosis. Similarly, ethylene glycol (antifreeze) is converted into glycolic acid, glyoxylic acid and oxalic acid by aldehyde dehydrogenase, lactate dehydrogenase (LDH) and glycolate oxidase Accumulation of the end product, calcium oxalate causes significant kidney injury.
For the purposes of reviewing how environmental chemicals and chemical mixtures interact with mucosal membranes in the body I will focus on the lung, due to its large surface area,and the intimate association between its air spaces and the vasculature and lymphatic systems. The lung itself faces several significant challenges due to its role and structure.
- Epithelial cells lining airways and alveoli are not highly exfoliative, requiring specific cellular regeneration & repair after serious damage.
- The large tidal volume of inhaled air daily increases encounters with a broad range of toxins and toxicants.
- The branching and narrowing of airways tends to trap particulate matter.
- Lung immune cells (macrophages, neutrophils) can produce lung injury via inflammatory mediators and reactive oxygen species (ROS)
- Potential damaging ROS generation is also potentiated by the High pO2 in this compartment.
The lung also varies significantly in structure and cellular composition throughout its length from the nose to the terminal air spaces. In the upper airway, the predominant cell type is ciliated columnar epithelial cells, interspersed with mucus secreting cells. The airways are covered by a layer of fluid and mucus that is constantly being propelled ‘upwards’ by cilia from the distal to proximal lung airways, from where it is ultimately swallowed. Within the upper airways, such mucociliary clearance is a key innate defence mechanism that protects the airway from harmful inhaled agents. If mucociliary clearance is impaired, the excess mucus forms plugs that promote bacterial colonisation of the airways. These highly specialised cells are therefore critical to the health and function of the pulmonary system.
The respiratory zones of the airways include the respiratory bronchioles and alveoli. The airway wall in the respiratory zones of the airways is much thinner, promoting gaseous exchange. Type I pneumocytes cover more than 98% of the alveolar surface, characterised by thin cytoplasmic extensions to form the air-blood barrier essential for normal gas exchange. Type II pneumocytes Type II are smaller, characterised by apical microvilli and lamellar bodies containing a surfactant within their cytoplasm. They have four main functions: (1) the production and secretion of surfactant to reduce surface tension in the lung; 2. Regulation of innate immunity and secretion of immunomodulatory proteins; 3. Regulation of solutes and 4. Regeneration of alveolar epithelium after injury.
Overlaying this epithelium is a thin aqueous layer derived from secretions from the underlying cells and movement of plasma proteins. This extracellular compartment has been studied in detail through the use of a variety of sampling techniques, including nasal lavage, bronchial wash and bronchoalveolar lavage. In these procedures areas of the airway are washed with saline and the recovered fluids analysed for both cellular and acellular components. These investigations have shown this compartment to contain high levels of antioxidants, with low molecular weight sacrificial antioxidants, to limit the generation of reactive oxygen species, but also metal chelation proteins and enzymatic antioxidants. In addition, a range of anti-inflammatory and microbicidal proteins and peptides have been identified in this compartment demonstrating that the lung lining fluids play a critical role in preventing oxidative stress and suppressing inappropriate immune responses.
The composition of the extracellular fluids has also been shown to vary throughout the length of the respiratory tree reflecting the unique cell populations within each of the regions. For example, mucus components and lactoferrin (an iron binding protein) being evident in the more proximal airways, with surfactant proteins and glutathione being more abundant in the distal lung.
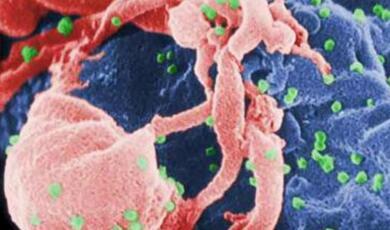
Thus far we have only considered the structural cells at the air lung interface, but a wide range of white blood cells are also found at the airway surface, as well as within the submucosa that play roles in the elimination and detoxification of foreign material, antigen presentation, tissue repair and remodelling. Inflammatory cell populations also vary throughout the airway with macrophages dominantly in the distal lung and neutrophils being more plentiful in the upper airways.
Understanding the regional differences within the airway is important as depending on the chemical physical properties of inhaled chemicals, particles or fibres they will deposit differentially within the airway. For example, more water-soluble gases, such as SO2 will be absorbed in the upper airway, whilst poorly soluble gases such as NO2 and O3, will penetrate further into the airway. The deposition of particles in the lungs is governed by sedimentation due to gravity, Brownian diffusion, and impaction by inertial force. Larger particles (> 10 μm) are generally retained in the oropharyngeal region and larynx due to impaction and are then swallowed representing an underexplored oral exposure route. Particles between 2 and 10μm normally deposit in the tracheobronchial region, with particles between 0.5–2μm are deposited in the alveoli and small conducting airways. Deposition is minimal for particle diameters in the range of 0.1–1.0μm, where particles have minimal sedimentation or impaction and are sufficiently large so as to have minimal diffusive deposition. Another factor relevant to understanding the toxicology of inhaled xenobiotics is the effective tissue dose at their sites of deposition. As the distal lung has a significantly greater surface area than the conducting airways, doses tend to be reduced within this compartment.
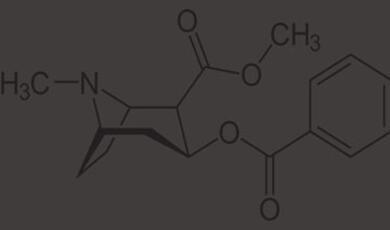
Given the focus in this series of lectures on population level exposures to harmful chemical toxicants it would be impossible to omit the elephant in the room. Whilst attention in the literature has focused on emerging chemical concerns there is a very real risk that we take our attention off the major inhaled toxicant known to cause significant health burdens globally, namely cigarette smoke. Whilst the combination of education, regulation and taxation has significantly driven down smoking in the UK, this trend is not evident in every country globally. In the UK, in 2021, 13.3% of people aged 18 years and over smoked cigarettes, which equates to around 6.6 million people in the population; the lowest proportion of current smokers since records started in 2011.
Cigarette smoke is a complex aerosol of gases and particulates. There are approximately 600 ingredients in cigarettes, which when burned creates more than 7,000 chemicals, many of which are established toxins, Cd, As, Pb, benzene, formaldehyde, NO2 etc. Each cigarette smoked is sufficient to cause injury to the airways, with both immune and structural cells at the surface of the lung driving acute inflammatory responses, which over time result in significant changes in tissue morphology. However, to place this process in context it’s important to understand the endogenous responses occurring at the airway surface, in relation to the magnitude of the challenge. The model is overly simplistic, but it implies that at low levels of stress tissues respond predominately in an adaptive mode, upregulating antioxidants and proteins involved in the detoxification, or sequestration of toxicants. As the stress increases, the adaption becomes insufficient and response tip first toward first inflammation and ultimately cell injury.
There are a few complications here about cigarette smoke. One of the key transcription factors that mediates the response of tissues to environmental stressors is the aryl hydrocarbon receptor. Polycyclic aromatic hydrocarbons (PAHs), are ubiquitous environmental toxicants, present within cigarette smoke, and known aryl hydrocarbon receptor (AHR) ligands. Activation of the AHR leads to upregulation of cytochrome P450 (CYP) metabolising enzymes which are generally important for the biotransformation of toxicants to less toxic intermediates, but in the case of PAHs their metabolism results in more toxic intermediates.
As above not all tissue adaptations themselves are beneficial in the long term. Epithelial cells at the surface of the lung exposed to stressors can undergo a range of tissue adaptation, some of which provide short term benefit. For example, cigarette smoke inhalation is associated with hyperplasia and metaplasia of the bronchial airway epithelium. This results in a more robust barrier to the inhaled toxicants, but makes the airway more prone to recurrent infections, due to the loss of ciliated epithelial cells and hyper mucus secretion. Similar effects can be seen in the upper airways of individuals exposed to air pollution, as exemplified by changes in the nasal mucosal architecture seen in an immigrant arriving into highly polluted Mexico City.
These adaptations over time are associated with a loss of lung function, though there is evidence that smoking cessation can stem the rate of functional decline. The consequences of cigarette smoking are marked, significant years of lost life, extended periods of disability related to a plethora of smoking related diseases: heart disease, lung cancer, COPD (bronchitis and emphysema). Again, it is important to reflect on the fact that whilst we discuss, and rightly so, the impact of air pollution on health, the impacts of cigarette smoking are still greater, as was highlighted in the analysis within the six Cities study which we covered in the last lecture.
Finally, I wanted to reflect on what happens when the barrier is breached. The lung has often been described as a leaking bucket allowing exchange of solutes with the vasculature. With both smoking and air pollution there is clear evidence of extra-pulmonary effects, though it is still much debated whether this is driven by particles, or particle associated chemicals entering the circulation, or the overspill of inflammatory mediators from the lung into the microcirculation. In the former case there is experimental evidence demonstrating this, but it is only likely to be a very small proportion of the total inhaled dose. Most inhaled particles will likely be eliminated by the mucociliary elevator, or intercepted by phagocytic cells in the lung and there is definite evidence to support this.
There is clear evidence of particle accumulation in the human lung both due to smoking and air pollution (in non-smokers). Airways lavages of smokers retrieve large numbers of heavily pigmented macrophages, even in ex-smokers, suggesting that these cells have resided in the tissue for extended periods of time. Recent data from the USA looked at draining lymph nodes from humans and found evidence of particle accumulation in an age dependent manner. Particulates were specifically contained within a sub-population of macrophages, which exhibited decreased activation, phagocytic capacity, and altered cytokine production compared with non-particulate-containing macrophages, suggesting that they may contribute to compromised immune surveillance of the lung.
So, what have we learnt over these three lectures? Our environment significantly impacts our health, and this is not only a correlation. There is increasing evidence of causal pathways to acute and chronic disease. We have evolved robust mechanisms to detoxify, eliminate and regulate responses to inhaled toxicants, but increasingly our protective barriers are exposed to chemical classes that we did not evolve alongside, and we may see unexpected interactions, such as between the AhR and PAHS. Given that our biology is immutable, it is important that we continue to emphasise the need to regulate and understand society’s chemical emissions. Our lung, our other barriers, will strive to protect us, but we must understand this comes at a longer-term biological cost.
© Professor Mudway, 2023
Part of:
This event was on Mon, 27 Mar 2023
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham College plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login