Christopher Wren’s Medical Discoveries: the ‘Architect of Human Anatomy’
Share
- Details
- Text
- Audio
- Downloads
- Extra Reading
** Please note that this lecture will contain several mentions of early animal testing which some audience members may find upsetting**
Christopher Wren was part of probably the first ‘research team’ assembled in Oxford in the 17th century, dedicated to better understanding the human body. With colleagues, Wren contributed to: the near-discovery of oxygen; the first human transfusion of blood; the first intravenous therapy and first intravenous anaesthetic; the description of the anatomy of the arteries supplying the brain (the ‘circle of Willis’); and remarkably, the first successful cardiac resuscitation.
The lecture will explain the continued relevance of these discoveries.
Download Text
Christopher Wren’s Medical Discoveries:
The ‘Architect of Human Anatomy’
Professor Jaideep Pandit
17th May 2023
Introduction
Christopher Wren (1632-1723) was an architect, astronomer, and mathematician, and his links to Gresham College are well known. In this lecture I will focus on his contributions to biomedical science, in particular his discoveries that have led to, or are connected with practical advances in the field of medicine, through some important discoveries but more notably, through the way he presented and depicted his own research findings and that of others. It is notable that when we consider these contributions, we should be reminded that he was not a trained physician.
Sources
In entitling a lecture or piece about an individual, and especially one of the stature of Wren, it is important to avoid hagiography. Whilst it is possible to ascribe many of the researches below to ‘Wren’, one of the most fascinating aspects of the period and place where he worked – Oxford in the mid-1600s - was that the scientific outputs should really be seen as those of the world’s first ‘scientific research group’. Several of this group (Robert Boyle 1627-1691 and Robert Hooke 1635-1703) went on to found the Royal Society, coincidentally after a lecture by Wren at Gresham College (28 Nov 1660). Others of the Oxford group included Richard Lower (1631-1691), John Mayow (1641-1679) and Thomas Willis (1621-1675). In the background was William Harvey (1578-1657), whose discovery of the circulation of blood influenced so much of this group’s work.
Thus, Jones (1958) catalogue’s references to Wren’s medical works from a long list of original sources, piecing together references to Wren’s contributions in publications by many other colleagues. Doerr (1985) writes that “Wren's notes were few, and he gladly allowed others to borrow his ideas or inventions, without attribution…Wren's contributions were significant in his own right…[he saw the need for a co-operative attack on problems]…, and especially through his ideas, discoveries, or pieces of apparatus cheerfully appropriated by contemporaries like Hooke and Boyle…”
In other words, it is not the intention of this lecture to claim ‘Wren did X’ – or indeed to overlook the possibility or fact that ‘Wren did Y’, but rather to emphasise the scientific content and relevance for today of what Wren and his contemporaries were undoubtedly collaborating on and discussing together.
I offer Wren’s contributions under five main headings: anatomy (including brain anatomy and the Circle of Willis); intravenous drug, fluid and blood administration; lung function; resuscitation, and finally some general contributions.
Anatomy and The Circle of Willis
Anatomical dissection was perhaps the primary means of experimental investigation of the human body in that era (sophisticated scientific equipment commonplace today being sparse), and new discoveries were constantly being made by simple but careful observation. Anatomists began to classify tissue according to its type (e.g., bone, muscle, nerves, vessels) and slowly began to relate type to function. One reason why progress was slow was the state of the body at the time of dissection: issues of preservation of the corpse, and the manner of death. The more violent the death, or invasive the disease that cause death, the more aberrant would be the resulting anatomy reported at post mortem, and hence uncertainty around what a ‘normal’ structure would be. As far back as Galen in 2nd century AD it was known that there was (probably) a network of small arteries at the base of the brain termed the rete mirabile (wonderful net), but Figure 1 below shows how imperfectly they were described and reproduced in art.
The Oxford group, led by Thomas Willis, had several advantages in their approach. First, access to a corpse whose anatomy was not deranged by trauma. A Wadham College undergraduate, Samuel Mashbourne died after being struck by lightning on 10th May 1666, whilst out on the river. Described by John Wallis, Willis found the body perfectly preserved other than some superficial burns to the skin (electrocution does not damage deep tissues, as we now know). Second, Willis aided by Wren combined anatomical dissection with some experimental science by injecting the blood vessels with dye, better to delineate their course. This built on (or helped develop) intravascular injection techniques first described by Wren (discussed below). Third, the resulting diagrams relied greatly on Wren’s expertise as a draftsman. Figure 2 shows how the brain has been drawn through the ages, the attempts reflecting what was interpreted by the anatomist performing the dissection. Wren’s depiction (Figure 3) is arguably less true to what is actually seen, but being more ‘architectural’ with its lettering and labelling offers a clearer functional interpretation; i.e., we can use Wren’s drawing as a map.
The functional significance of the circle of Willis, now well established but also self-evident from Wren’s illustration, is that it provides a means by which blood flow to the brain can be maintained even if one of the main arteries supplying the brain becomes blocked or damaged. Blood supply to the brain is via four vessels: the paired carotid and vertebral arteries. If there was no ‘circle’ linking these, then block or severance of any one would result in death of the entire part of the brain supplied by that vessel (i.e., approximately one quarter). The circle facilitates continued blood flow to that part of the brain, via the remaining patent vessels. In terms of evolution: it was a significant evolutionary advantage to develop and retain a circle connecting these vessels, because the cost or risk of not having one was too great.
This advantage of the circle of Willis is relied upon in modern day surgery. Carotid endarterectomy is surgery to remove plaque from the carotid arteries, which can otherwise cause narrowing and reduce blood flow to the brain, leading to a stroke, or a ‘mini-stroke’ (transient ischaemic attack’). During surgery, the carotid artery has to be clamped to stop blood flow and allow the surgeon to work on the vessel – but without a well functioning circle of Willis this clamping itself could cause a stroke. One challenge is then how to know the circle of Willis is working well, when the patient is under general anaesthesia? (It is not possible to diagnose stroke in an already-unconscious patient). While there are several technical solutions relying on measuring pressures and flows in the vessels, another approach is to perform the operation awake, under local/regional anaesthesia. Any reduction in brain blood flow with clamping will result in change in the patient’s cognitive function, speech, or movement of limbs. My own work has helped describe the effective ways of providing the local anaesthetic (Pandit et al., 2000), as well as the underlying anatomy that makes these blocks effective (Pandit et al., 2003); Figure 4.
Intravenous Access
Equipment Design
There were several preliminary ideas that led to the concept of the intravenous route as access for drugs and fluids into the body. The first was Harvey’s discovery of the circulation of blood in the early 17th century. The predominant theory before that was that blood ‘ebbed and flowed’ to and from the heart, with blood in the veins and arteries mixing. This theory relied upon the existence of holes within the heart that permitted this mixing of venous and arterial blood. However, Harvey (and earlier anatomists like Vesalius) were unable to find any such pores: the septum of the heart completely separates the right and left sides of the heart. A second key discovery was valves within the large veins that made it impossible for blood to flow backwards: the only direction for blood to flow along the veins was towards the heart. Harvey elegantly combined these anatomical observations with a simply physiological study, that can be repeated by anyone, anywhere (Figure 5).
A second was Boyle’s idea of turning poisons into medicine as a means of new drug design. In a part-published “An Essay of Turning Poisons into Medicines” (Hunter, 2009), Boyle turned on its head Paracelsus’ dictum that “All things are poison, and nothing is without poison; the dosage alone makes it so a thing is not a poison”. Paracelsus, a German physician (1493-1541), had noted that all drugs are fundamentally alike and it is only the dose administered that matters. Boyle reasoned that if all beneficial drugs could be poisonous in overdose, poisons could be used to advantage at the correct, lower dose.
The third development was Wren’s design of a method (in essence a quill) to cannulate blood vessels, through which substances could be injected. Designing an intravenous catheter is not straightforward: the tip needs to be sharp enough to pierce the vessel but wide enough to permit injection of fluid; the length short enough to minimise resistance to flow, but long enough to handle; and the diameter large enough overall to keep the catheter in place, perhaps with flanges or wings that can be held, stitched or taped in place. The early design was a single canula that both pierced and permitted injection; modern day designs separate the two functions (Figure 6). Having designed the original equipment it seems Wren handed over much of the later experimental work to Lower and Boyle (Rivera et al., 2005; Dorrington and Poole, 2013). Nevertheless, his central role is depicted in a painting by Ernest Broad (1877-1934; an artist who specialised in early historical portraits); Figure 7.
The technique of intravascular access permitted, as discussed above, delineation of arteries in the circle of Willis. It also led to the first intravenous anaesthetic, drug administration and blood transfusion, as discussed below.
The First Intravenous Anaesthetic
The Oxford team obtained intravenous access in a dog by Wren first making an incision in the hind limb, exposing and then ligating the vein distally. A brass plate then immobilized the vein (describing the cannula as “more than half an inch long and about one-quarter of an inch wide, with sides bending inwards; almost of the shape and bigness of the Nail of a Mans Thumb, but somewhat longer, it had four holes near the corners for fastening to the vessel by threads, and contained along most of its length a slit through which the vein could be incised with a lancet from the Ligature towards the Heart, great enough to put in at it the slender Pipe of a Syringe”). As Dorrington and Poole note, the use of the word ‘syringe’ is intriguing, as a syringe connectable to an intravenous cannula was not reported until much later in the 19th century (Figure 6). So it is possible that the team (possibly Wren) also designed a syringe, whose design is now lost, or that the bladder attached to the canula (Figure 5) was being referred to as a syringe. The team administered a mixture of opium and alcohol and observed the dog to become unconscious: “[the tincture] getting into the mass of Blood . . . was quickly, by the circular motion of That, carry’d to the Brain…before the Opium began to disclose its Narcotick Quality…and presently after [the dog] appear’d so stupifi’d…”.
In essence the team had performed the first intravenous anaesthetic in an animal. Importantly, the dog recovered to full health, so this anaesthesia was reversible. There are several notable aspects of Boyle’s use of language above. First, the appreciation that blood, being in circulation, is able to carry elements around the body. Second, the appreciation that the action of the opium-alcohol tincture is on the brain. Third, that there follows ‘narcosis’; a term now used interchangeably with ‘anaesthesia’.
Although Boyle entertained using the intravenous route for other therapies, notably emetics, the team never developed the idea of anaesthesia. Etherisation via inhalation was described much later in the mid-19th century and intravenous anaesthesia was not again used until the introduction of thiopentone in the 1930s. Intravenous anaesthesia had an advantage. Inhalational induction of anaesthesia was not only slow, but after initially becoming sedated, the patient entered a paradoxical stage of excitability in which they could suffer muscular spasms, bite their tongue, vomit or suffer laryngeal spasm (known as Guedel’s ‘stage 2’). The speed of induction by intravenous anaesthesia avoided this dangerous stage. However, there was a downside discovered when thiopentone was used for anaesthesia in surgery for injuries oin soldiers after the Pearl Harbour attack in 1940. It is said that thiopentone killed more US servicemen than the Japanese bombs, because the need to administer intravenous fluid before anaesthesia had not been appreciated. The rapid effect of anaesthesia on the brain, noted by Boyle and Wren, also had a similar immediate and depressive effect on the heart and circulation, such that these patients, being already hypovolaemic with blood loss, soon lost their blood pressure.
The combination of intravenous alcohol and opiate – Boyle and Wren’s mixture – was reported as recently as the 1970s by authors arguing it was an ideal combination in surgery using heart-lung bypass. In this situation, inhalational anaesthesia is ineffective (the bypass machine diverts blood away from the lungs, so it cannot absorb anaesthetic), and at the time the other commonly available anaesthetic agents had either too long-lasting an effect, or too depressive an effect on the heart and circulation. The authors argued that alcohol and opiate presented the ideal combination (Dundee, 1970; Mannheimer, 1971). Other drugs (e.g., propofol) are now used, making this combination (at last) redundant.
Blood transfusion
Richard Lower developed Wren’s technique for vessel cannulation and focussed on blood transfusion. He was convinced that aeration of the lungs gave arterial blood its rich red colour, and without such aeration, life could not be sustained. He experimented on asphyxiating and bleeding animals to support this notion. He was describing what we now understand to be oxygen uptake within the lung (see also the work of Mayow, below), and oxygenation of haemoglobin in the blood. The next logical step was that blood from a healthy donor could then help a sick patient, if it was transfused. Developing Wren’s original instruments (e.g., the cannulae needed to be larger to permit effective flow of blood; Figure 8), he first successfully performed transfusion between two dogs (and other animals; including a demonstration at Gresham College), then progressed to transfusing blood from a sheep into a ‘harmless lunatic’ in the hope of improving the patient’s mental condition. The patient survived, but was apparently no less insane (Donovan, 2004).
In fact, Lower was beaten to the first human transfusion by Jean-Baptiste Denis in Paris. Although transfusion became popular for a while, very soon (unsurprisingly), deaths were reported (the first in a patient of Denis’) and the treatment became banned by law. It only became properly established on a firm scientific footing after discovery of blood groups and understanding of transfusion reactions in the 20th century.
Function of the Lungs: Near-Discovery of Oxygen
Wren’s first interest had been in the way muscles worked, and he developed a theory that there was an ‘explosion’ within them as the basis for contraction (“Dr. Wren made use of this experiment to explain the motion of the muscles by explosion"; Bennet, 1976). This is close to the modern idea that cellular respiration is a form of ‘combustion’. Further, Wren realized there must be a link between the air, as providing a ‘vital constituent’ to the muscles for their ‘explosion’. He described (in writing rather than in a diagram) an instrument that could recycle exhaled air, such that it was purified and re-breathed, without need for fresh air, speculating that a chemical could remove any undesirable properties within the air, permitting it to be re-breathed (Bennet, 1976). Remarkably, he was describing here a system commonly used in anaesthesia to deliver oxygen to the patient. Soda lime scrubs the exhaled air of carbon dioxide, permitting it to be rebreathed by the patient: thus a low flow of oxygen can be used and the system saves on gas use (Figure 9).
A member of the Oxford team, John Mayow, was interested in the composition of the air, and what the lungs actually did. Older theories of the lungs ascribed functions such as warming (or cooling) the air, storing blood, helping heart to pump, or purifying air (or blood) in some manner. Thinking and interpretation were constrained by phlogiston theory, which held that all combustible substances contained an element phlogiston, released when burned. Phlogiston was toxic (perhaps closest to CO2) and dephlogisticaed air was pure and could be breathed. The phlogiston theory predicted that, if as Wren proposed, muscle action was a form of explosion or burning, then the volume of air exhaled should increase with muscle activity.
Mayow conducted a series of experiments (Figure 10) in which small animals or burning objects were placed inside upturned flasks over water. To his surprise, the level of water inside the flask rose – the volume of air diminished, as if something was being taken from the air – rather than dropped. This was contrary to the prediction from phlogiston theory. We now know that it is oxygen (O2) being absorbed by the body that reduces the volume of the air in the flask. Normally, this is replaced by a near-equivalent volume of CO2 but impurities in the water almost certainly caused CO2 to dissolve, fortuitously giving the result. Moreover, the similarity of the result with animals and burning coal implied that combustion (respiration) was indeed at the root of biological processes. Although Mayow promoted the idea of ‘nitro-arial particles’ as being taken from the air, his language and interpretation was not so clear as to overturn phlogiston theory, elements of which he tried to retain.
It was left to Antoine Lavoisier, in Paris, much later in late 18th century to discover and name oxygen, based on observations that metals gained weight (through oxidation) rather than lost weight as predicted by phlogiston theory. He was also able to extract and purify oxygen.
Cardio-Pulmonary Resuscitation
All these researches in anatomy, intravenous medication, transfusion, lung function, and oxygen culminated in the most remarkable act of the world’s first documented cardiac resuscitation. Before the 17th century, there had been random descriptions of how the apparently dead might be revived. They could not be based on any rational interventions because what is needed for successful cardiopulmonary resuscitation (CPR) is knowledge of (a) what the heart does and how it works, and (b) what the lungs do and how they work. Harvey in describing the circulation, had pari passu implied that the heart is a pump, driving the circulation. In his experiments leading up to transfusion, Lower had both ventilated the lungs of a recently-dead animal with air, whilst compressing the heart manually, and found that the blood leaving the lungs became red, as in a vivisection of a living animal. Unwittingly, he had performed the first CPR in an animal. Mayow had come close to discovering oxygen, or at least concluded something like nitro-aerial particles were extracted by the body from the air, via the lungs. And Wren had described an intravenous method for rapid administration of drugs. Thus, whilst not articulated in modern language, all the ingredients for successful CPR (lung ventilation, cardiac compression and drug administration) were known to the Oxford team.
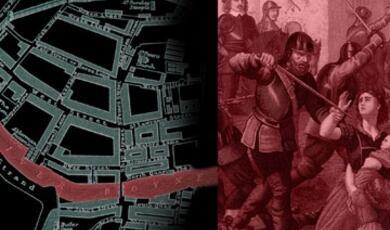
Anne Green, a maid, suffered a late miscarriage but concealed the foetus’ body. This being discovered, she was quickly arrested, tried and hanged (Figure 11). (It seems that the pregnancy was the result of her being seduced, or raped, by the grandson of her distinguished employer, Sir Thomas Read). As was customary, Thomas Willis as Professor of Anatomy, along with an Oxford physician William Petty (who also served as Gresham Professor of Music), claimed the body and dragged it to Willis’ home in Beam Hall (where the Oxford team conducted many of their experiments). For whatever reason – perhaps Anne coughed, or perhaps they were simply moved to apply their results in practice – Willis and Petty started to resuscitate her (Hughes, 1982). A contemporary note deposited in the Bodleian Library confirms that “[the body…] was carried to the colledge of physitians, where all the learned doctors and chyrurgions met..” (A Declaration from Oxford, 1651). Given that Anne remained there for several weeks this suggests that the whole team including Wren, not just Willis and Petty, were likely involved. It is unclear what was done, but probably all of drug administration, artificial ventilation, cardiac compression, and perhaps other measures like warming and feeding helped in successful resuscitation. The justices of peace, feeling ‘the hand of God had preserved her’ granted a pardon, and Anne left to live in the country, apparently taking the coffin in which she had been placed. The family charged people to view or meet her, and by now being well off, married, bore three children, and lived for another 15 years.
Other Contributions
Microscopy
While Wren is better known as an astronomer, viewing the stars, he also made early and key contributions looking the other way, as it were, in microscopy (Gest, 2005). Wren helped design a microscope and collaborated with Robert Hooke to publish Micrographia, a work in which many of Hooke’s illustrations of magnified fleas and plants were modelled on similar diagrams by Wren, now part of the Royal Collection (Figure 12).
Operative Surgery
In his book 'Operation and Method of Cure', Wren focused on developing surgical techniques. Using the example of (probably) the first removal of the spleen in a dog, he described how to use anatomy to produce excellent results, tie vessels to minimize bleeding, avoid pitfalls (such as damaging the intestine or handling delicate tissue too harshly) and especially emphasized careful postoperative care to ensure recovery. It is unclear why Wren chose the spleen, but modern indications for splenectomy include trauma, tumours, enlarged spleen (due to many other causes, the enlarged spleen itself causing problems for the blood) or, blood disorders such as sickle cell anemia or thalassemia.
Wren probably assisted Willis in either or both surgical operations or dissections and his illustration of an intestine with a typhoid ulcer (Figure 13) is extraordinary for its beauty: without knowing what it is, it could pass for dyed cloth from an exotic country.
Hospital Design
Wren applied his architectural skills to design hospitals and medical institutions. Amongst these are the Royal Hospital, Chelsea; the King William, Queen Mary and Queen Anne Courts of Greenwich Hospital; possibly the Royal Hospital Kilmainham in Ireland; and the College of Physicians, Warwick Lane, London (destroyed in 1866); Figure 14.
Concluding Remarks: Some Personal Links
I am not a Wren scholar. My interest stems from various ‘points of connection’ with his work, and that of the 17th century Oxford team. One, discussed above, is my work in improving effectiveness of local blocks for awake carotid artery surgery. This relates to the Circle of Willis, for which Wren provided the illustrations. As an anaesthetist, I work closely with colleagues applying the surgical techniques described by Wren in his book on operative surgery.
A second link is to Wren’s work with Mayow on oxygen and respiration. The circle system that I use as an anaesthetist (Figure 9) is exactly the equipment Wren described as providing pure air for rebreathing. Mayow’s equipment that could have led him to discover oxygen (Figure 10) was developed further by CG Douglas in the early 20th century as a ‘Douglas bag’ (Figure 15). The bag collects expired air and the O2 and CO2 content can be analysed to provide information on metabolic rate. If the CO2 is scrubbed, then the volume of the bag declines in proportion to O2 consumption by the body, in exactly the same way as the volume of air in Mayow’s inverted flasks. Douglas (1882-1963) was Tutor in Physiology at St John’s College, Oxford – succeeded by RW Torrance (1923-1999) – who in turn I succeeded. Thus, for over 100 years since the start of the 20th century, just three of us – with that direct link to early work on oxygen – have taught Respiratory Physiology at St John’s.
Third, St John’s connects in a most unexpected way, and one irrelevant to medicine. Wren’s father (also Christopher) studied at St John’s, and somehow got to sign a window in the college’s Old Library (Figure 16).
Finally, many of the experiments described in this essay, much of Wren’s biomedical work in Oxford, and the resuscitation of Anne Green were undertaken in the rooms of Thomas Willis in Beam Hall. Built in 1187, this has the distinction of being the oldest, continuously inhabited university building in the world (Figure 16). The connection in this regard is that I had the honour of being allocated Willis’ rooms when an undergraduate at Oxford in the 1980s, and I find it continually remarkable and inspirational that all these things happened in my rooms, with so many of these scientists gathering to discuss and experiment all those years ago.
© Professor Pandit 2023
References and Further Reading
A declaration from Oxford https://ota.bodleian.ox.ac.uk/repository/xmlui/handle/20.500.12024/A82084#
Bennett JA. A note on theories of respiration and muscular action in England c. 1660 (Christopher Wren). Medical History 1976; 20: 59-69.
Doerr AH. Ars Scientia: Scientia Ars (Obverse and Reverse Sides of the Coin of Genius: Leonardo da Vinci and Sir Christopher Wren). Journal of Thought 1985; 20: 59-69.
Dumitrescu AM, et al. The discovery of the circle of Willis as a result of using the scientific method in anatomical dissection. Romanian Journal of Morphology & Embryology 2020; 61: 959-965.
Donovan A. Richard Lower, M.D., Physician and Surgeon (1631–1691). World Journal of Surgery 2004; 28: 938–945.
Dorrington KL, Poole W. The first intravenous anaesthetic: how well was it managed and its potential realized? British Journal of Anaesthesia 2013; 110: 7-12.
Dundee JW. Intravenous ethanol anaesthesia: a study of dosage and blood levels. Anesthesia and Analgesia 1970; 49: 467–75.
Gest H. The remarkable vision of Robert Hooke (1635–1703): first observer of the microbial world. Perspectives in Biology and Medicine 2005; 48.2: 266–72.
Gibson WC. The bio-medical pursuits of Christopher Wren. Medical History 1970; 14: 331-41.
Hughes JT. Miraculous deliverance of Anne Green: an Oxford case of resuscitation in the seventeenth century. British Medical Journal 1982; 285: 1792-3.
Hunter M. Boyle. Between God and Science. New Haven: Yale University Press, 2009; 106
Jones HW. Sir Christopher Wren and natural philosophy: with a checklist of his scientific activities. Notes and Records of the Royal Society of London 1958; 13: 19-37.
Mannheimer WH. The use of morphine and intravenous alcohol in the anesthetic management of open heart surgery. Southern Medical Journal 1971; 64: 1125–7.
Molnár Z. On the 400th anniversary of the birth of Thomas Willis. Brain 2021; 144: 1033-1037.
Neher A. Christopher Wren, Thomas Willis and the depiction of the brain and nerves. Journal of Medical Humanities 2009; 30: 191-200.
O'Connor JP. Thomas Willis and the background to Cerebri Anatome. Journal of the Royal Society of Medicine 2003; 96: 139-43.
Pandit JJ, Bree S, Dillon P, Elcock D, McLaren ID, Crider B. A comparison of superficial versus combined (superficial and deep) cervical plexus block for carotid endarterectomy: a prospective, randomized study. Anesthesia & Analgesia 2000; 91: 781-6.
Pandit JJ, Dutta D, Morris JF. Spread of injectate with superficial cervical plexus block in humans: an anatomical study. British Journal of Anaesthesia 2003; 91: 733-5.
Rivera AM, Strauss KW, van Zundert A, Mortier E. The history of peripheral intravenous catheters: how little plastic tubes revolutionized medicine. Acta Anaesthesiologica Belgica 2005; 56: 271-82.
Wallis, J. A relation of an accident of thunder and lightning at Oxford. Philosophical Transactions of the Royal Society 1666; 1: 222-226.
Wickens AP. Five depictions of the brain. The Psychologist 2017; 20: March.
References and Further Reading
A declaration from Oxford https://ota.bodleian.ox.ac.uk/repository/xmlui/handle/20.500.12024/A82084#
Bennett JA. A note on theories of respiration and muscular action in England c. 1660 (Christopher Wren). Medical History 1976; 20: 59-69.
Doerr AH. Ars Scientia: Scientia Ars (Obverse and Reverse Sides of the Coin of Genius: Leonardo da Vinci and Sir Christopher Wren). Journal of Thought 1985; 20: 59-69.
Dumitrescu AM, et al. The discovery of the circle of Willis as a result of using the scientific method in anatomical dissection. Romanian Journal of Morphology & Embryology 2020; 61: 959-965.
Donovan A. Richard Lower, M.D., Physician and Surgeon (1631–1691). World Journal of Surgery 2004; 28: 938–945.
Dorrington KL, Poole W. The first intravenous anaesthetic: how well was it managed and its potential realized? British Journal of Anaesthesia 2013; 110: 7-12.
Dundee JW. Intravenous ethanol anaesthesia: a study of dosage and blood levels. Anesthesia and Analgesia 1970; 49: 467–75.
Gest H. The remarkable vision of Robert Hooke (1635–1703): first observer of the microbial world. Perspectives in Biology and Medicine 2005; 48.2: 266–72.
Gibson WC. The bio-medical pursuits of Christopher Wren. Medical History 1970; 14: 331-41.
Hughes JT. Miraculous deliverance of Anne Green: an Oxford case of resuscitation in the seventeenth century. British Medical Journal 1982; 285: 1792-3.
Hunter M. Boyle. Between God and Science. New Haven: Yale University Press, 2009; 106
Jones HW. Sir Christopher Wren and natural philosophy: with a checklist of his scientific activities. Notes and Records of the Royal Society of London 1958; 13: 19-37.
Mannheimer WH. The use of morphine and intravenous alcohol in the anesthetic management of open heart surgery. Southern Medical Journal 1971; 64: 1125–7.
Molnár Z. On the 400th anniversary of the birth of Thomas Willis. Brain 2021; 144: 1033-1037.
Neher A. Christopher Wren, Thomas Willis and the depiction of the brain and nerves. Journal of Medical Humanities 2009; 30: 191-200.
O'Connor JP. Thomas Willis and the background to Cerebri Anatome. Journal of the Royal Society of Medicine 2003; 96: 139-43.
Pandit JJ, Bree S, Dillon P, Elcock D, McLaren ID, Crider B. A comparison of superficial versus combined (superficial and deep) cervical plexus block for carotid endarterectomy: a prospective, randomized study. Anesthesia & Analgesia 2000; 91: 781-6.
Pandit JJ, Dutta D, Morris JF. Spread of injectate with superficial cervical plexus block in humans: an anatomical study. British Journal of Anaesthesia 2003; 91: 733-5.
Rivera AM, Strauss KW, van Zundert A, Mortier E. The history of peripheral intravenous catheters: how little plastic tubes revolutionized medicine. Acta Anaesthesiologica Belgica 2005; 56: 271-82.
Wallis, J. A relation of an accident of thunder and lightning at Oxford. Philosophical Transactions of the Royal Society 1666; 1: 222-226.
Wickens AP. Five depictions of the brain. The Psychologist 2017; 20: March.
Part of:
This event was on Wed, 17 May 2023
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham College plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login