Coronary Heart Disease
Share
- Details
- Text
- Audio
- Downloads
- Extra Reading
Coronary heart disease caused by narrowing and blockage of the heart arteries causes angina, heart attacks and heart failure. It remains one of the commonest causes of mortality in the UK and globally. Public health interventions and improvements in treatment have steadily reduced deaths from coronary heart disease.
This lecture will discuss the causes of coronary heart disease and advances in reducing its effects.
Download Text
Coronary Heart Disease
Professor Chris Whitty
10th January 2022
The heart is an extraordinary organ which everyday pumps around 100,000 times. It provides oxygen to all other organs and removes waste. It is very responsive to increase in need, increasing when there is a need for physical or other activity. It keeps blood pressure and flow optimised. It is therefore essential to all other organs of the body.
The function of the heart had not been realised when this college was founded in 1597. William Harvey’s discoveries about the flow of blood around the body published in 1628 were the first new understandings. Since then, the heart and its diseases has been one of the most studied areas of medicine and this series will cover only some of the extraordinary advances that have been made.
There are three main groups of things that can lead to the heart failing or stopping. The first, covered in this lecture, is myocardial ischaemia; lack of oxygen to the muscle of the heart usually due to narrow or blocked coronary arteries. The other two are that the heart rhythm goes too fast or too slow; and the structure of the heart, including muscle or valves, may be damaged; ischaemic heart disease can also contribute to both of these. These are considered in subsequent lectures. This note lays out the themes covered but is not a transcript of the lecture.
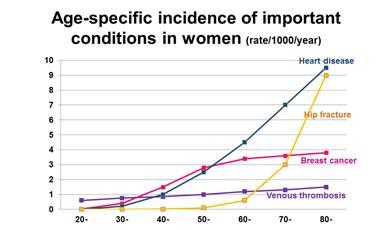
Ischaemic disease, also often known as coronary heart disease, is the second leading cause of recorded mortality in UK and the commonest worldwide. Of this, the most common cause of death is myocardial infarction (MI) commonly called a heart attack.
Although heart and circulatory disease still cause around a quarter of deaths, this is a major improvement since the early 1960s when it caused about half of deaths in the UK. At that point it substantially exceeded deaths from all cancers and infectious diseases. Mortality from ischaemic heart disease has continued to decrease although the decrease has slowed since around 2014 in the UK, based on steadily improving science translating into prevention and treatment.
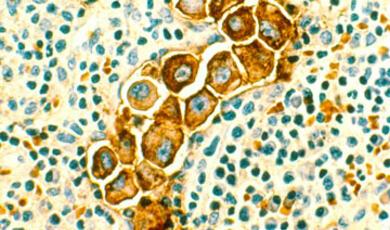
The most important cause of ischaemic heart disease is atherosclerosis. Fatty deposits mainly caused by cholesterol causing a narrowing of the arteries of the heart which gradually build up over a lifetime. They can cause critical narrowing causing angina due to reduced oxygen to heart muscle. Rupture of the plaque can cause a clot which blocks the blood vessel, and this is a common cause of heart attack (MI). There are however many modifiable risk factors which if addressed can lead to a delay of many years before ischaemic heart disease has its effects or in some cases prevent it altogether.
Broadly prevention of deaths from heart disease can be divided into three groups. The first is primary prevention, generally things the State or society does to reduce risk to everybody in society irrespective of their pre-existing disease. The next is secondary prevention, which is reducing the risk to an individual who has early disease or a specific risk factor, usually in consultation with a healthcare worker such as a doctor. The final mechanism is treatment which reduces mortality including from heart attacks, and also reduces symptoms and subsequent risk.
Primary Prevention
Primary prevention of ischaemic heart disease includes: reducing smoking and second-hand smoke (passive smoking); reducing air pollution; reducing salt and some fats in food; making it easier to exercise; reducing societal drivers of obesity.
Smoking is the most avoidable cause of premature mortality from heart and circulatory disease. It drives a lot of the difference between the areas of the UK with the highest mortality from heart disease and the lowest, especially in younger people. Caused entirely by a small number of companies making massive profits generally from the poorest in society by addicting them at the youngest possible age, the heart disease caused by smoking is essentially entirely preventable. Improvements in heart disease are often very rapid when smoking reduces. Bans on smoking in public places were followed by a significant reduction in coronary admissions, often within weeks. It needs to be stressed that what keeps most people smoking is addiction where the choice has been taken away from them by aggressive marketing of a highly addictive product at an early age. Most smokers wish to quit; addiction prevents them. Smoking is falling in all age groups in UK but encouragingly most rapidly in young adults. The harmful effects of smoking on cardiovascular disease will however be a significant driver in the UK and most other countries for the foreseeable future.
The next major driver which is a societal problem is air pollution, in particular particulate matter. People underestimate how much air pollution drives cardiovascular disease. Most forms of air pollution have been falling rapidly over the last 50 years, but there is a significant way they could go further and this would further reduce the risk of heart disease in the general population.
One important way to improve heart health, and indeed most health, is exercise. Making exercise easy and fun throughout the life course so that it becomes widespread will lead to significantly reduced cardiovascular mortality. Starting with interventions such as the daily mile in schools, through the working age, for example through making active travel by walking or cycling easier, and onto interventions in older age, such as walking football, are some of the many ways to encourage people to take exercise and enjoy it as part of their daily life.
High blood pressure is one of the biggest drivers of heart disease, and one of the modifiable causes of this is high levels of salt in the diet. Salt increases blood pressure, and the elderly are particularly salt sensitive. There has been steady improvement in reductions in salt in many products but there is a long way to go. Only 18% of salt in UK diets is added by choice; the rest is added during manufacture or is naturally present and people have no choice about how much they take and are unaware they are doing so.
Finally, among the drivers of heart disease which require a societal response considered in this lecture is obesity. There has been a steady increase in people living with overweight and obesity from 15% in 1993 to 28% of the adult population. Rising obesity starts in childhood especially in the most deprived areas and tackling childhood obesity should be seen as a societal priority for multiple health reasons. It is possible to intervene in a way which works with people’s lives, an example of which was the sugar levy on soft drinks.
Secondary Prevention
Secondary prevention, for which there are a number of definitions, includes targeted help for individuals for those who need it due to particular risk factors. This might include targeted help for an individual to stop smoking, lose weight, or increase their exercise. It also includes treating hypertension, high cholesterol and diagnosing and treating diabetes.
High blood pressure, also known as hypertension, is a major, common cause of ischaemic heart disease. It contributes to about half of heart and circulatory disease. Around 28% of UK adult population has hypertension which increases with age. Fortunately, there are multiple possible treatments; the key is to diagnose it early and treat it. Blood pressure is easy to measure including at work, home, the shops and by a doctor. High blood pressure is usually 180/90 mm Hg or higher. Sometimes this can be reduced through lifestyle changes, including reducing salt intake or alcohol consumption, increasing exercise and losing weight; even a little helps.
Many drugs can reduce blood pressure by different mechanisms. Which one is best for an individual person depends on age, existing heart disease, diabetes, ethnicity, and side effects among other issues. These risks and benefits will be discussed between the individual person and their doctor or other healthcare worker. Common drug classes include ACE inhibitors, angiotensin II receptor blockers, calcium channel blockers, thiazide like diuretics and beta-blockers. These may be used in combination. The lecture goes through each of these in more detail.
Reducing cholesterol where people have high levels also reduces and delays heart disease. The mainstay for this is reducing fats in the diet, and statin drugs which bring down LDL cholesterol. New classes of drugs collectively termed PCSK9 inhibitors are now coming into clinical practice.
Treatment of symptomatic ischaemic heart disease and heart attacks.
Even with optimal prevention many people will have cardiac symptoms or events (but significantly fewer than without prevention). Broadly the conditions or events can be divided into myocardial infarction (heart attack), angina and unstable angina.
Angina occurs on exercise or other stress of the heart, typically with chest, jaw or arm pain although other symptoms such as shortness of breath may occur. It is usually predictable in the sense that the same level of exercise will provoke it and it goes away on resting.
Myocardial infarction (heart attack) and unstable angina is usually signalled by chest pain or tightness or other severe symptoms that occur or continue at rest. They are a medical emergency. Sudden shortness of breath, clamminess, dizziness and nausea are other possible symptoms; not everybody has chest pain although it is the most common symptom people notice.
The most important thing is to exclude a heart attack or treat it early. Three things help diagnose myocardial infarction (MI); symptoms and history including age; ECG; blood tests in particular troponin.
If someone has typical symptoms for MI there are broadly three outcomes. The first is it is assessed not to be from the heart (there are other, potentially serious, non-cardiac causes of chest pain, although many are not dangerous).
If a myocardial infarction is diagnosed with ST elevation on ECG this usually leads to rapid transfer to cardiac centres for angiography, where the patient will be assessed for emergency stenting, or drugs which break down clots.
If the troponin is raised but the ECG is normal or shows more limited changes it is usually termed a non-ST elevation myocardial infarction (NSTEMI). Someone may have typical symptoms, but troponin blood tests and ECG does not show heart attack; this would be normally termed unstable angina. Although there is an important difference between unstable angina and NSTEMI as the myocardial infarction has led to heart muscle damage, for treatment they are broadly managed the same way.
Almost any person with suspected myocardial infarction will receive aspirin and another drug which aim to reduce platelet function and therefore reduce clotting at the site of the heart artery narrowing. They may in ST elevation MI (STEMI) receive either emergency angioplasty where the clot is removed or bypassed with a stent or a thrombolytic (clotbusting) drug.
Coronary stenting (angioplasty) has revolutionised the management of a lot of angina as well as myocardial infarction. The stent, which can usually be placed into an artery in a short procedure, leads to a widening of the narrowing in the coronary artery. An alternative surgical approach is coronary artery bypass grafting (CABG). CABG is a major operation where the chest is usually opened requiring several days in intensive care or hospital beds but in the right patient is highly effective. Which is the better option will need discussion with cardiologists and surgeons.
Following either significant angina or a heart attack several drugs are usually given to prevent, delay or reduce future problems. These include antihypertensives if someone is not already on them, reducing cholesterol with statins, drugs acting on the neuro-hormonal system including beta-blockers and ACE inhibitors, and antiplatelet drugs such as aspirin.
One more class of drugs worth considering as it is important for symptoms is nitrates. These been recognised as a treatment for angina since the 1870s. They relax coronary and other arteries. Short-acting GTN drugs usually given as a spray or a tablet under the tongue are useful rapid relief of angina symptoms. Long-acting forms can also be used to reduce symptoms.
Although most people think of angina as inevitably caused by narrowing of the large blood vessels of the heart, not all angina is in fact due to atherosclerosis of coronary arteries. Some angina with normal coronary arteries can be due to microvascular angina and coronary artery spasm. Treatment for angina depends on the cause.
Important mechanisms by which heart disease can occur are inflammatory conditions. Inflammation is for example thought to be one of the ways in which air pollution increases cardiovascular risk. Many infections are known to increase the risk of acute coronary events including myocardial infarction and generally the more severe the infection the higher the risk and the longer the excess risk.
The remarkable improvements in cardiovascular mortality and morbidity from ischaemic heart disease are due to multiple incremental improvements. Primary prevention including on smoking, air pollution and exercise have a significant impact. Secondary prevention including antihypertensives and statins reduce the probability of disease. Treatment of myocardial infarction and other ischaemic heart disease has improved considerably, leading to much better outcomes. Many of the trends on cardiovascular diseases are in the right direction including reduced smoking. There are however several headwinds including rising obesity and consequently rising diabetes. Ischaemic heart disease remains one of the major killers in the UK and globally and there is much we can do to improve it even with existing science whilst researching new ways to combat it.
© Professor Whitty 2023
Part of:
This event was on Tue, 10 Jan 2023
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham College plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login