Diseases of the Heart Structure, Muscle and Valves
Share
- Details
- Text
- Audio
- Downloads
- Extra Reading
The normal heart is very robust. Some people are born with abnormalities of the heart structure. Others acquire damage to the heart valves which become too narrow or unable to close properly. The muscle and linings of the heart may be affected by infections, drugs or other inherited or acquired diseases. All of these can cause heart failure or death if not treated.
This lecture will consider the prevention and treatment of structural heart disease.
Download Text
Heart Disease
Diseases of the Heart Structure, Muscle and Valve
Sir Chris Whitty
16th May 2023
This third lecture in a series on diseases of the heart considers damage to and disease of the structures of the heart- the muscle, valves and pericardial covering of the heart. The two previous lectures considered two other major groups of abnormalities which can lead to heart failing: myocardial ischaemia (coronary heart disease) and arrhythmia where the heart rhythm is either too fast or too slow. These notes indicate the issues that are being discussed in the lecture but are not a direct transcript.
The understanding of the structure and function of the heart changed around the time Gresham College was founded in 1597. The anatomy of the heart had been described and recorded many times including by Leonardo da Vinci, and in a very important study of anatomy by Andreas Vesalius published in 1543. There was however much debate and misunderstanding about its function with a critical turning point being William Harvey’s work published in 1628 demonstrating the circulation of blood around the body.
We now know the heart is effectively two pumps in one with four chambers which circulate the blood around the body. The left side of the heart pumps blood around the main organs of the body and the right side pumps blood through the lungs. The heart is mainly made up of a strong and relentless muscle usually contracting once a second or more. The blood flows in one direction because of two sets of valves; when the atrium contracts from the atrium into the ventricle and then when the powerful muscle of ventricle contracts from the heart into the circulation. Around the heart is a fibrous covering, the pericardial sac. This lecture will consider the more common things that can go wrong with these three elements; the heart valves, the heart muscle and the pericardial sac.
Diagnosing structural heart disease has several elements. After understanding the history including symptoms, doctors will undertake a physical examination of the heart size, pulse and blood pressure. Heart valve problems also make typical noises and a major advance was the stethoscope. This was first developed in Paris in 1816 and subsequently improved in stages. Plain chest x-ray for heart size and shape and ECG (discussed in more detail in the lecture on arrhythmia, where it is the central diagnostic test) also provide useful information.
The confirmation of diagnosis of structural problems of the heart is now undertaken with various forms of imaging. Most common is cardiac ultrasound and Doppler, often called an echocardiogram. The cardiac ultrasound gives a non-invasive dynamic picture of the structure of the heart including the muscle wall, valves and the space around the pericardial sac whilst the Doppler component measures flow across valves and any leaks. This is most commonly done across the chest wall (transthoracic) but it can also be done from behind the heart in the oesophagus, as stress echocardiogram, or occasionally in the heart. Advances in a cardiac MRI and CT radiography mean these are also used, particularly in more complex cases.
Heart valves- acquired valvular heart disease: stenosis, regurgitation and endocarditis.
The heart valves functioning normally are central to keep the blood flowing in the right direction at the right pressure. For the left side of the heart, the mitral valve controls the flow from the atrium to the ventricle, and the aortic valve from the ventricle to the body. On the right side, the tricuspid valve controls the atrium to ventricle flow and the pulmonary valve the ventricle to the lung. Damaged valves may either become narrowed, known as stenosis, or floppy or partially open known as regurgitation, or both. Minor stenosis or regurgitation of all 4 valves is relatively common as people age but clinically important valvular heart disease is most commonly on the left side of the heart (mitral and aortic).
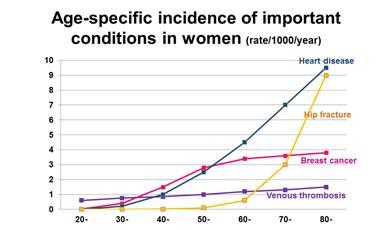
At this point of time the great majority of acquired valvular heart disease is in older people and usually is degenerative-calcific. Age is the major risk factor but high lipids, hypertension, diabetes or obesity, chronic kidney disease and smoking are all risk factors in common with coronary heart disease.
Many people who have valvular heart disease have no symptoms, at least initially. As disease progresses, symptoms may include shortness of breath doing activities people are used to, dizziness or fainting especially on exercise, chest pain, fatigue and swelling of the limbs or abdomen.
The second set of diseases of the valves of the heart are infections with bacterial or fungal growths on the heart valves, known as endocarditis. Endocarditis is rare but serious, with risk factors including having artificial valves and congenital heart abnormalities. Risks for bacteria getting into the blood include intravenous lines for people in hospital, recreational intravenous drug use, dentistry or surgery. Some bacteria such as Staphylococcus aureus have a particular tendency to cause endocarditis but different bacteria may occur if the cause is dental, gut damage or the patient is immunosuppressed. Endocarditis is treated with antibiotics or antifungals depending on the infecting organism. Sometimes surgery is needed.
Historically, a very important cause of acquired valvular heart disease was rheumatic heart disease. Rheumatic fever follows a Group A streptococcal throat or skin infection. It used to be very common in the UK in the pre-antibiotic era. It is an immunological reaction rather than the infection itself that can damage the heart valves, in particular the mitral valve. It remains a risk globally in areas where people are living in poverty.
Initial treatment of symptomatic valvular heart disease may be medical with drugs. Drug treatment does not cure valve problems but may control the symptoms sufficiently that people can continue their normal lives. These may include rhythm control, blood pressure control and diuretics to reduce fluid build-up.
Severe acquired valve disease may however need surgery. Wherever possible, surgeons will use valve repair rather than valve replacement. This is more common in mitral than in aortic valve disease. Repair has the advantage that it is your native valve so there is lower risk of clots or infection. The most minimally invasive is a balloon valvuloplasty where a balloon is used to stretch the valve if it is narrowed. This is a relatively minor procedure but usually only works for a limited period.
Most valve repairs and replacements will still require open-heart surgery. The standard method requires the sternum (breastbone) to be split. The circulation is put on a bypass machine and the heart is stopped temporarily to allow the surgeons to do their work after which the heart is restarted. Replacement valves have steadily improved. They were initially a ball and cage valve. There are now a variety of tilting discs and fibrous valves including from humans or animals. Which one is best depends on age amongst other factors.
Some centres now use less invasive surgical methods to replace or repair valves with several cuts to the chest and leg used to undertake the operation. If patients are at high anaesthetic risk (high chance of death or serious outcome during the operation), a TAVI procedure- transcatheter aortic valve implantation- can be used for aortic stenosis. A catheter is inserted into the groin and advanced to the heart where an artificial valve is fixed over the existing valve. This can be done under local anaesthetic.
Valve surgery is major surgery with risks as well as benefits, but it has been transformative. Many people who would have died or lived very constrained lives have had the quantity and quality of their lives significantly improved.
Heart muscle damage- cardiomyopathy and myocarditis.
Cardiomyopathy is damage to the heart muscle. Three main types occur. The most common is dilated cardiomyopathy. This is most commonly due to heart attacks (myocardial infarction) or other ischaemic damage. Hypertrophic cardiomyopathy is usually inherited. Restrictive cardiomyopathy is where the heart muscle becomes inflexible often due to infiltration.
Common symptoms of cardiomyopathy are similar to several other forms of heart disease. These include shortness of breath especially on exercise, fatigue, dizziness or lightheadedness on exercise, swelling of the feet or legs, arrhythmia or chest pain.
Ischaemic dilated cardiomyopathy is the most common form in high income countries. Prevention and early treatment are the same as for coronary heart disease, covered in the first lecture in the series. Hypertension is particularly important to control. Several drugs and toxins can also damage the heart muscle causing dilated cardiomyopathy. These include alcohol in large quantities over time, cocaine and amphetamines, some chemotherapy drugs, and some chemicals used in industrial processes including lead, mercury and cobalt.
Dilated cardiomyopathy during or just after pregnancy is very rare but important. It usually occurs late in pregnancy or the first few weeks after delivery and the cause is unknown. Most women recover completely but this may be slow, and a minority are left with significant problems.
Hypertrophic cardiomyopathy (HCM) is usually inherited as an autosomal dominant condition. It can occur at any age but most commonly begins in late teens to early adulthood. All first degree blood relatives should be screened as it can be associated with sudden deaths especially in athletes (but this is exceptionally rare).
Restrictive cardiomyopathy where the heart muscle becomes more rigid and less able to contract can be caused by infiltration or scarring. Causes, most of which are rare, include haemochromatosis with too much iron in the body, sarcoid, amyloid, connective tissue diseases and some drugs and radiation.
A temporary form of cardiomyopathy is stress-induced, sometimes known as broken heart syndrome. This sudden myocardial dysfunction after a stressful event such as bereavement or divorce. This can lead to severe heart dysfunction but is temporary (days to weeks).
The end result of cardiomyopathy if it progresses is likely to be heart failure. Not all heart failure is due to cardiomyopathy but it is an important cause. It can be from mild to severe. Treatment of heart failure depends on severity. All risk factors which might lead to further progression need to be addressed including smoking, blood pressure and cholesterol. ACE inhibitors and beta blockers are the first-line treatment. Mineralocorticoid receptor antagonists such as spironolactone may be used if people still have symptoms.
In more severe cases, a range of drugs and procedures will be considered to optimise remaining cardiac function. Specialist clinics will usually use a combination of drugs and it often takes some time to get the balance of drugs right, including their positive effects and their side effects. If there are rhythm disturbances pacemakers, cardiac resynchronisation therapy devices and implantable defibrillators may be needed. Coronary artery stents and coronary artery bypass surgery may also be needed if, as is commonly the case, there is coexisting ischaemic heart disease.
In some very severe cases, heart transplants or an artificial pump in the heart may be used. Heart transplants are rare with around 100-150 a year performed in the UK. They need a good match since there are many risks including graft rejection, graft failure and reaction to the drugs which are used after the event. In selected people however they are transformative with most people alive at least five years later and half surviving at least 10 years.
Geographically much more localised but important in that area is a parasitic disease called Chagas disease passed on by biting bugs in specific areas of Latin America. This is still the most common cause of non-ischaemic cardiomyopathy in Latin America but rates are fortunately falling.
The heart muscle may become inflamed. This is myocarditis. Most people with myocarditis recover fully but it is an important cause of heart disease in young adults and children and occasionally can cause sudden deaths. The most common causes for it are viral infections including Coxsackie B, Parvovirus B19, HIV, Hepatitis C and COVID-19. Several bacteria can also cause it including Legionella, mycoplasma and brucellosis. There may be some initial inflammation due to the infection directly, and in some a second immune inflammation. Vaccines can rarely cause myocarditis but generally at much lower rates than the infection they are protecting against.
Historically, a very important cause of myocarditis was diphtheria. Here it is not an infectious or immune response but the toxins from diphtheria that damage the heart muscle and cause myocarditis. Diphtheria is now rare due to a combination of better living conditions, antibiotics and vaccination.
Non-infectious myocarditis can be caused by several inflammatory conditions. These include the autoimmune conditions such as sarcoid or lupus, some drugs and vaccines and some environmental toxins. All are rare.
Most myocarditis is a one-off event, and people recover.
The pericardial sac- pericarditis and pericardial effusion.
Pericarditis is inflammation of the pericardial sac covering the heart. Patients with it normally make a full recovery between a few days or a few weeks, although occasionally it can take months. It is seldom very dangerous on its own although there are some exceptions. It can cause rhythm disturbances and often occurs with myocarditis. The symptoms are chest pain, often sharp and stabbing, worse on lying down or taking a deep breath.
The most common causes or pericarditis are viral infection including ‘flu and COVID-19. Other infections including bacterial, tuberculosis and fungal diseases along with inflammatory diseases like rheumatoid arthritis can cause pericarditis. It can occur after heart attack or heart surgery, with some drugs and vaccines, and due to blunt trauma to the chest.
A pericardial effusion is fluid building up between the heart and the outer layer of the pericardial sac. Many conditions can cause a small pericardial effusion which usually resolves. In some cases however, this can become a very serious threat. Haemorrhage into the pericardial sac following heart wall rupture after heart attack or surgery is an emergency. The classical cause of a slower onset massive pericardial effusion is tuberculosis, although other inflammatory causes and cancers can also cause it. It can lead to squeezing of the heart known as cardiac tamponade, also a medical emergency.
Congenital valve and heart structure conditions.
Prof Martin Elliott has delivered lectures on this at Gresham College available online so I will cover this important topic only briefly. Congenital heart problems are relatively common with just under 1% of births in high income countries having some form of congenital heart abnormality. Of these around one in four are critical but many of them are clinically relatively unimportant or self-correct as the child matures. Ventricular septal defect and atrial septal defect (‘hole in the heart’) are the most common.
Holes in the heart often self-correct early in life or are minor and require no intervention. Patent ductus arteriosus (PDA) may close after drug treatment. Some larger holes in the heart can now be closed via a catheter inserting a closure device; this is a relatively minor procedure. Some more major congenital cardiac abnormalities however need surgery, sometimes in stages or at particular points in a child’s development.
In summary, abnormalities or diseases of the cardiac valves, muscle and pericardial sac are important causes of mortality and morbidity everywhere. They need to be tackled by a combination of prevention, drugs, devices and surgery.
© Chris Whitty, 2023
Part of:
This event was on Tue, 16 May 2023
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham College plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login