Sexually Transmitted and Intravenous Infections
Share
- Details
- Text
- Audio
- Downloads
- Extra Reading
Some diseases are specialised in using sexual behaviour for transmission. Major pandemics including HIV and syphilis have been transmitted via this route, along with the cancer-causing infections Hepatitis B and HPV. Along with these are highly transmissible diseases such as gonorrhoea and herpes. Another way people share bodily fluids is via needles, and several diseases can be transmitted this way, including HIV and Hepatitis. Changing sexual behaviour is hard, so other methods have to be found to control these diseases.
Download Text
This lecture is part of a series looking at the major routes of transmission of infectious diseases and considers two linked routes of transmission: sexual and blood to blood (bloodborne). Although these two seem quite different several major diseases are both sexual and blood-borne infections. Previous lectures have been on vector borne and oral routes of transmission. Later lectures will consider transmission of other respiratory and touch routes. The theme of the series is that usually one route of transmission dominates for any infection, although a secondary (or more than one secondary) may occur. It is essential to understand this route because the behaviour of diseases and their control depends on the route of transmission. These notes are just an outline of the themes of the lecture and not a transcript.
Other infectious routes of transmission can be between strangers at a distance. Oral infections can be passed up the food chain or down the river many miles. Mosquitoes might transmit an infection acquired in one village in another. By contrast sexually transmitted infections (STIs) are almost always transmitted by close contact with someone the infecting person knows, loves, cares deeply about or desires. Several viruses, bacteria and parasites have evolved to take advantage of human desire for intimacy, love and sexual contact. This is a potentially efficient transmission strategy. Social contact involves very close prolonged and often repeated contact in relatively less defended parts of the body. The gut for example has multiple layers of defence against infection; mucosal surfaces of the genital area much less so.
It is often assumed STIs are medically trivial, and some are, but many are not. Several major diseases are transmitted mainly by the sexual route. These include HIV; syphilis; several infections which cause cancer; causes of infertility stillbirth and neonatal damage. Even those with relatively small physical impacts can cause stress and relationship damage.
Medicine’s ability to intervene between an infectious person and the person potentially infected are different from other routes. When the chain of transmission is long there are multiple places where it can be broken. Waterborne diseases can be prevented by improving water supply; vector borne diseases can be combated by attacking the vector before it can infect someone. By contrast STI’s (and intravenous drug use) evolve contact that is direct and personal. There is therefore much greater reliance on case finding and early treatment. Misplaced embarrassment and shame are a major reason people do not seek help early for these common diseases. For medical staff diagnosing and treating STIs is normal business. Stigma is a major barrier to diagnosing and treating STIs, and their wider control. Behaviour changes to reduce transmission is possible, for example greater use of condoms. For some important STI’s we now have vaccines. For many however treatment remains the mainstay of protecting individuals and preventing transmission and this requires early diagnosis. Because some people find it difficult several different routes are available for people to discuss and to be diagnosed with STI’s; these include general practices, specialist clinics and hospitals but also separate and entirely confidential sexually transmitted infection clinics for those who prefer complete anonymity. Identifying treating STIs is important for you and for any sexual partner.
Unsurprisingly STIs are mainly diseases of sexually active adults. This is in contrast to most other infectious diseases which have the greatest impact on the very young and older and very old adults. STIs generally occur, if at all, after sexual debut so are usually diseases of adulthood and since they are most commonly acquired before people have formed long-term partnerships tend to be most common in younger adults. Many if untreated can however remain infectious for years or even for life. People are often unaware they are infected, as many people have minimal or no symptoms. The first time they may be aware they are infected is when a new sexual partner gets symptoms- sometimes from a disease which may have been acquired years previously (including more than one partner ago).
A particularly important time of life for these infections is in those who are pregnant or wish to become pregnant. Several STIs are a threat to fertility in women and men. Some major STIs can be passed vertically from mother to baby including HIV, syphilis and Hepatitis B. Some can be passed to the baby in the birth canal during labour causing problems such as blindness. Checking for STIs and treating them before or during pregnancy should therefore be seen as normal good care.
Blood-borne infections are transmitted blood to blood. Historically the most important route was probably medical practice using the same needle or knife on more than one person. Blood products were also high risk before effective screening for infections was introduced. These medically transmitted infections have massively reduced as a result of disposable needles, sterilisation and screening of blood products. Now the blood-to-blood route is mainly intravenous drug users (IVDUs) sharing needles. Major blood-borne infections for intravenous drug use and STIs overlap: HIV, Hepatitis B and Hepatitis C. This is a serious route of transmission and reducing it through interventions such as needle exchanges is an important part of public health.
Donating blood is an extraordinary gift from one person to another they (usually) do not know. It can be lifesaving. It can also transmit infections. To reduce the infection risk, some temporary exclusions from giving blood including when people are themselves unwell, or where they have recently travelled to countries with particular infections (for example where malaria is common as malaria can occasionally be transmitted blood to blood). Through these measures and screening the blood itself for infections such as HIV and Hepatitis C infections via this route are now exceptionally rare.
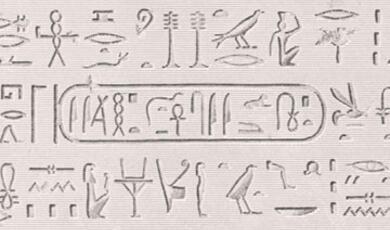
The rest of the lecture considers individual diseases of importance which are transmitted primarily by the sexual route, with in some cases an important blood-borne secondary route. The first is syphilis. Syphilis was a new disease to Europe in the 1490s, although its original origins are still debated. It was realised fairly early on that it was sexually transmitted and quickly blamed on foreigners- for example in England called the French disease, in other countries called the Italian or Spanish disease and so on. As a disease which caused serious illness, visible scars and had social stigma it was widely feared. It had a profound effect on the practice of medicine.
Syphilis is a major multisystem disease which can cause serious damage to many parts of the body. Primary syphilis involves a painless ulcer lasting a few weeks soon after acquiring infection. This is followed by secondary syphilis with fever, generalised rash and various ulcers. Many years later if untreated tertiary syphilis can cause serious damage including to the brain, nerves, eye, bones, joints, skin, heart, great blood vessels and liver.
As the new disease was not known to Galen and Hippocrates it allowed a major rethink of medical theory and practice. It changed the relationship between surgery and medicine allowing surgeons to expand their practice. It led to the conversion or building of hospitals or wards including ones near this College and had a significant impact on society (and literature).
Syphilis remained a very major and common disease until the end of the pre-antibiotic era. Around 10% of adult male Londoners in 1919 had it. It is one of the commonest causes of dementia at that stage. The first really effective treatment, Salvarsan, appeared in 1910 based on arsenic. It was the introduction of penicillin which largely collapsed the epidemic in high income countries and prevents late complications. It also required a network of clinics to find cases and their contacts and treat them.
Since the 1980s HIV/AIDS is one of the most severe new threats to health of our lifetime. Over 36 million deaths occurred to date. HIV was originally an infection of chimpanzees and other monkeys passed on to humans. It was identified in multiple ways in the early 1980s and at that stage had 100% mortality. HIV destroys key parts of the immune system mediated by CD4 cells allowing common infectious diseases, several rare fungal diseases and some cancers to kill the person infected. There are however many years between initial infection and the very serious damage to the immune system of aids during which affected individual can pass HIV on.
The HIV pandemic, the last really serious pandemic before COVID-19, was made up of several epidemics which overlapped and interacted. There was a large heterosexual epidemic in Africa and parts of Asia and worldwide which was the largest and caused the greatest number of deaths, and many children were infected from infected mothers. Much of the epidemic in Europe and North America occurred in men who have sex with men (MSM). There was additionally intravenous drug use (IVDU) epidemic and initially some blood products for example for treating haemophilia.
HIV spread very widely and most rapidly in southern Africa where in some communities up to 30% or more of the young adult population were infected. Since this caused almost inevitable mortality the impact on society as well as individuals was dramatic. In the absence of medical countermeasures such as drugs and vaccines the initial response had to be trying to change social behaviour, which is not easy. Probably the most important initiative was the promotion of condoms and other barrier methods of contraception.
The real transformation came with the development of drugs to treat HIV- the HAART era. The first serious antiretrovirals were from the mid-1990s. Initially they were moderately effective with significant side effects, very expensive and complex to take. They became steadily simpler, more effective, safer and importantly cheaper since so much of the burden of disease and mortality was in lower income countries. As a result of these drugs life expectancy for HIV-infected people is now broadly similar to non-infected if rapidly diagnosed and treated.
As a result of these drugs mortality from HIV AIDS has been steadily dropping globally. They also have an important effect in reducing transmission. The chances someone with HIV who is well controlled on HAART passing on HIV onto a partner is close to nil. The drugs can also be used as preexposure prophylaxis. They are important in controlling the mother to child transmission if women are infected during pregnancy.
The lecture now turns to sexually transmitted infections which cause cancer. The first is human papilloma virus (HPV) of which there are many types but a few which cause cancers. These viruses are very common and often caught very early in sexual life. Some HPV can also cause genital warts which can be distressing but are not dangerous. HPV causes cervical cancer, one of the most common cancers in young women. The introduction of an effective HPV vaccine is leading to substantial drops in cervical cancer rates in the vaccinated, on top of the important role of screening for it. It is likely that globally HPV, and therefore cervical cancer rates will drop significantly over the coming years. HPV can also cause a number of other cancers, mostly transmitted sexually including penile, anal and throat cancers and these also should be combated by the vaccination programme.
Hepatitis B and C are sexually and bloodborne infections which cause significant rates of cirrhosis and liver cancer around the world. Hepatitis B is the more common and is easy to catch. Transmission between adults is sexual, or via IVDU. There can then be vertical transmission mother to child and then horizontal (bloodborne) transmission between children with most infection before the fifth year. There are drugs to suppress but not cure hepatitis B but there is now highly effective vaccine deployed worldwide and this very important sexually transmitted cause of cancer will become much less common over the next decades. Hepatitis C is largely blood-borne with some sexual transmission component. There is no vaccine but in the last 10 years several highly effective oral drugs are being used and can cure it before cirrhosis and cancer occurs if diagnosed early.
The next part of this lecture considers some common STI’s. The first is gonorrhoea. This is much less serious than HIV or untreated syphilis but unpleasant and occasionally serious with complications such as joint infections. It is particularly high risk in pregnancy. It is quite common with around 35,000 cases diagnosed a year in the UK. Historically it has been treated by antibiotics but there is an increasingly serious problem with multidrug resistant gonorrhoea. In common with many other STI’s they can cause pelvic inflammatory disease and reduce fertility. It can also cause preventable miscarriage or premature labour and potentially blinding conjunctivitis of babies at birth so is important to address before or during pregnancy. It is currently increasing in incidence in the UK largely driven by an epidemic among men who have sex with men (MSM).
Chlamydia is another very common bacterial STI. Over 70% notice no symptoms and those who do notice pain when urinating, pain during sex or bleeding after, bleeding between periods and lower abdominal pain. It is important to identify and treat chlamydia. In women it can cause pelvic inflammatory disease and infertility and infect children during childbirth. In men it can cause epididymal and testicular pain, affect fertility and in men more than women (although both) lead to a form of arthritis lasting weeks to months.
Trichomonas is another common treatable sexually transmitted infection caused by a parasite. Only 30% of people have symptoms. In common with some other STI as it increases the risk of this with HIV being transmitted. It can be treated.
Genital herpes is rather different and is a very common viral STI. Oral herpes caused by HSV-1 (herpes simplex virus) is not passed on sexually and is acquired in childhood causing recurrent cold sores on the lips, although occasional sexual transmission can occur. HSV-2 is however a specifically sexually transmitted infection and causes the great majority of genital herpes. The first episode can be very unpleasant although not in everybody. Once it is acquired however, like cold sores it hides in the nerves and will re-emerge multiple times over a lifetime. This means that, in contrast to the previous STIs discussed which once treated will not be passed onto any subsequent partners, herpes has the potential to infect any subsequent sexual partner, and this can cause significant relationship difficulties for some. Drugs can reduce the frequency and severity of attacks but not eliminate the virus at this stage.
Pubic lice, also known as crabs, are not dangerous. They have evolved to live in pubic hair and occasionally other hair on the body but do not live in the scalp and are completely different from the headlice most common in children. There is person to person normally in sexual contact and are easy to treat once diagnosed.
Some diseases which are not STI’s have sexual spread as a potentially important secondary route. Two recent examples are Ebola (normally touch transmitted) and Zika (vector borne). In men they both can have can be prolonged survival of the virus for months in the male reproductive tract and seminal fluid. This is long after the virus has been cleared from other parts of the body. As a result, they can re-establish an epidemic later in time via sexual spread, or travel over distance for example with a man acquiring Zika in Brazil transmitting to his sexual partner in the USA.
Sexually transmitted and blood-borne infections are important as public health challenges. Some are common. Some are life-threatening. Early diagnosis and treatment is essential and this requires reducing the stigma around them. HIV, syphilis and Hepatitis C have been transformed by treatment. Vaccines for HPV and Hepatitis B will have major impact on cancers. Antibiotics treat most common sexually transmitted bacterial infections although drug resistant gonorrhoea is an increasing problem. Safe blood products, medical practice and IVDU needle exchange are central to reducing blood-borne infections. We therefore do have significant countermeasures, but they are very different from those for the routes of transmission we have considered so far in this lecture series.
© Professor Whitty 2022
This event was on Wed, 12 Jan 2022
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham College plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login