Targeted Therapies in Oncology: The Future of Ovarian Cancer
Share
- Details
- Text
- Audio
- Downloads
- Extra Reading
Ovarian cancer, the most lethal gynaecologic malignancy in both the US and UK, provides an excellent model of analysis for recent developments in novel therapies in oncology.
This lecture explores the natural history of the disease and discuss its current practice patterns. In addition, there is a focus on progress and set-backs of new drug development in cancer research.
Dr Liz Han is a Distinguished Fulbright Scholar, University of Texas and Royal Marsden Hospital London.
This lecture was hosted in association with the Fulbright Commission.
Other lectures by Distinguished Fulbright Scholars can be accessed here.
Download Text
The future of ovarian cancer treatment
Dr Liz Han
16/11/2009
Thank you very much for this opportunity to be raising ovarian cancer awareness. I appreciate everyone coming out tonight.
My name is Liz Han, and I have spent almost the last 10 years studying ovarian cancer. I hope to give a current overview of the disease for the first 45 minutes, and leave the last 15 minutes for questions.
At the end of my talk, I hope that everyone will walk away with a solid understanding of ovarian cancer statistics, how and when patients are diagnosed with ovarian cancer. In addition, what are the currently available treatments. What are the rationales behind the treatments that we give.
And as we anticipate the future, what are the potentials for the latest drugs in targeted therapy? Do they have a role in the treatment of ovarian cancer? Most importantly, how successful are we in terms of treating cancer as a chronic disease such as diabetes or high blood pressure where patients are expected to live a long time?
More specifically, we will not only discuss ovarian cancer statistics in both the UK and US, we will perform a quick review of the pelvic anatomy. Hopefully, with our quick review, ovarian cancer staging will make a lot more sense.
Ovarian cancer diagnosis involves a degree of screening. Unfortunately, methods for effective and efficient screening in this particular cancer have been some what of a moving target. Furthermore, it is also worthwhile to explore the genetic aspects of ovarian cancer in terms of inherited germline mutations in the setting of BRCA 1 and 2.
From there, we will continue our discussion of what is the current standard of care in the treatment of ovarian cancer. What are the relevant factors that configure into our decision making process when the cancer comes back. And, what are the options when the cancer comes back?
I am sure that the audience today is a fairly self-selective group of motivated people who wish to learn more about oncology...
Nonetheless, this may still be the first time that you have heard the term 'targeted therapy'. Targeted therapy refers to the knocking down of proteins that are over-expressed by the tumor, and that the over-expression of these proteins plays an important part of tumor's malignant phenotype.
There are 2 main classes of targeted therapy: small molecule inhibitors and biologics. An example of a small molecule inhibitor can be a tyrosine kinase inhibitor that stops the intracellular actions of the overexpressed proteins. The biologics include monoclonal antibodies that target overexpressed tumor protein. Both tyrosine kinase inhibitors and biologics can be classified as anti-angiogenic therapy if the target is a protein that plays a role in tumor angiogenesis. The most developed agent in anti-angiogenic therapy is bevacizumab which is a humanized monoclonal antibody.
We will also be talking about PARP inhibitors which are examples of another small molecule inhibitors, and they have caused some excitement in cancer patients with BRCA mutations, and we will discuss why this is the case.
In closing, we will discuss the likelihood of treating ovarian cancer as a chronic disease. Moreover, how close are we to individualized care based on a systematic genomic analysis of tumors?
The life time risk for ovarian cancer is about 1 in 70. In the United Kingdom, there are over 65-hundred new cases diagnosed every year.
However, out of England, Wales, Scotland and Northern Ireland, it is Wales that has the most new cases of ovarian cancer per population. The reason is not readily apparent to me.
As in the US, cancer arising from the uterus is the most common malignancy of the female reproductive tract.
However, it is easy to see that based on these statistics, cancer of the ovary is by far the most lethal of all gynecologic cancers.
Now, for American women, ovarian cancer is the 5th most common cancer across all organ systems. The American Cancer Society estimates that there will be over 21-thousand new cases of ovarian cancer diagnosed in America in 2009.
However, ovarian cancer ranks 4th in cancer mortality with an estimated deaths of more than 14-thousand this year. In women, ovarian cancer deaths are only surpassed by cancers of the lung, breast and colon.
The graph on the right shows how we as physicians have fared over the years.
The plot at the bottom of the graph is our cure rate for ovarian cancer.
As you can see, the slope is not so steep... In other words, we haven't made huge progress in increasing our cure rate.
However, we do see that in terms of median survival time, the slope is a heck of a lot steeper, which means that patients with ovarian cancer are living with the disease longer. Now the question that we should be asking is why is that the case? Why have we made very little difference in cure rate?
Well, this is in part due to the fact that almost 75% of all ovarian cancer cases are diagnosed in the advanced stage, at stage III and IV. Because of this, most of the times, the cancer comes back, and there is typically a 10-26 months period of what oncologists call progression free survival and that is the time interval from diagnosis to when the cancer recurs.
For all stages of ovarian cancer, the overall survival is 44%. That is, 44% of women diagnosed with ovarian cancer will be alive in 5 year's time.
Now, let's take a quick review of the female pelvic anatomy.
Many vital organs reside in the pelvis. In the female, uterus is located centrally. Anterior to that, you have the bladder. Posterior to the uterus, you have the rectum or the large bowel. Superior or on top of the uterus, you will find loops of the small bowel.
The ovaries are highlighted here.
Epithelial ovarian cancer, which is the most common type of ovarian cancer, spreads mainly by tumor shedding from the diseased ovaries. These tumor cells are then carried over to the neighboring organs, mainly the large and small intestines by a clockwise physiological current.
To determine what stage it is, the patient undergoes surgery in order for a thorough exploration the abdomen and pelvis.
Staging actually makes a lot of sense. For stage one, the cancer is confined to the ovaries. The 5-year survival is quite encouraging at 90%.
For stage 2, the cancer has spread outside of the ovaries to the pelvis where the 5-year survival is 70%.
For stage 3, which is the most common stage where patients are diagnosed with ovarian cancer, the cancer has spread to the pelvis and the upper abdomen. As expected, with advanced ovarian cancer, the 5-year survival takes a precipitous drop to only 23%.
For stage 4 ovarian cancer, the cancer has spread to distant organs such as the lung or inside the liver, and again, the 5-year survival statistic is disappointing.
Now, do we understand ovarian cancer well enough to identify women who are at risk for developing the disease? On this slide, we have clinical factors on the left and their possible relationship to ovarian cancer. If their corresponding box falls to the right of the middle line, these clinical factors increase the risk of developing ovarian cancer. And conversely, if their corresponding box falls to the left of the middle line, these clinical factors offer protection from developing ovarian cancer.
For example, if you have either a BRCA1 or 2 mutation which means you have an inherited germline mutation in the BRCA 1 or 2 gene that is responsible for fixing any mistakes that the body makes during DNA replication. And because of this heterozygosity, meaning you inherited a mutated gene from either your mom or your dad but you still have a good one, you are more likely to develop cancers of the breast and ovaries.
Older age as well as a personal history of infertility will increase your risk for ovarian cancer. Nulligravida is the medical term for never been pregnant, and that also appears to increase your risk for ovarian cancer.
Now, let's take a look at what will protect you from ovarian cancer. Early parity means early age of giving birth, that appears to be protective. Previous history of having your uterus out or hysterectomy with bilateral tubal ligation also is protective. Bilateral tubal ligation or 'having your tubes tied' is interesting in light of the recent reports that ovarian cancer may in fact start in the fallopian tubes.
Lastly, prior oral contraceptive pill use is protective. In fact, it can reduce your risk of ovarian cancer by 50% if you use it for 5 years or longer. Recent reports also reveal that the protection lasts long after you stop taking the birth control pill.
Now, this slide further outlines the risk reduction offered by birth control use. R.R. stands for relative risk, and as you can see, the longer you stay on the pill, the better the protection against ovarian cancer. In fact, if you were to take birth control pill for longer than 10 years, you bring your risk of developing ovarian cancer down by 5-folds.
On the other hand, clomid is a common fertility drug used to induce ovulation. In a study where women who have never used this fertility drug are compared with women who used this drug, it is found that with prolonged use, greater or equal to 12 cycles, it may increase your risk of ovarian cancer by 7-folds.
Let me just point out 2 important details: clomid is never prescribed for that many cycles in today's world of reproductive assistance. Often times, it is used for only 3 cycles or less before the patient is moved onto something else as the drug is unlikely to be more effective with prolonged use. Furthermore, the effects of short term clomid use on ovarian cancer risk is inconclusive, at this time, no-one really knows for sure how it affects ovarian cancer when used only for brief periods.
Out of all the cases of ovarian cancer that is diagnosed every year, roughly 90% of the cases are sporadic and the remaining 10% is hereditary.
And out of the 10% that is hereditary, we can see that BRCA 1 and 2 mutations together make up about 90% of this. HNPCC is hereditary non-polyposis colorectal cancer which is formerly known as lynch syndrome. It is a mismatch repair gene mutation that predisposes one to cancers of the colon, uterine and sometimes, ovary as well. Together HNPCC and other single gene mutations make up the remainder 10%.
Now, let's focus on BRCA1 and 2 mutations for a minute. The risk of ovarian cancer increases with age so that by age 70, if you are a BRCA1 carrier, your chance of developing ovarian cancer is about half. It is less for BRCA2 carrier, nonetheless, these risks are still significantly higher than that of the base line population.
I should mention that the lifetime risk of ovarian cancer for the general female population is 1 in 70 or 1.4%. Therefore, even if you are looking at the 12% risk of developing ovarian cancer by 70, that is still 10 times more than the general population.
As you may recall, I stated that as gynecologic oncologists, we haven't really significantly improved the cure rate for ovarian cancer. We may have a better knowledge of who's at risk for ovarian cancer, but in terms of screening in the general population, it is still very much a work in progress.
In order to come up with a successful screening program for a particular disease, there are several assumptions that have to be met. First, is the disease severe enough?
The answer is yes because advanced ovarian cancer, for the most part, is lethal. However, if caught early enough, we can improve the outcome.
Unlike cervical cancer where there is a long precancerous phase called dysplasia, we are not sure whether ovarian cancer has a detectable pre-clinical phase.
And as I have stated before, ovarian cancer has a life time risk of 1.4%, it really is not as prevalent as other cancers such as breast cancer.
And importantly, can we devise a cost-effective and non-invasive technique for ovarian cancer screening? The answer, unfortunately, is no- not at the present time.
Without an acceptable screening program, is there anything recognizable to raise our suspicion for ovarian cancer?
Ovarian cancer often produces a constellation of vague symptoms where patients are often sent for a gastrointestinal evaluation before being sent to a gynecologic oncologist. In a recent published study, the authors prospectively followed women with complaints of pelvic and abdominal pain with a frequency of greater than 12 times a months, and found that the likelihood for ovarian cancer as the underlying cause is 19-fold for duration lasting less than 6 months and over 23-fold for duration less than 12 months.
Other significant factors also include persistent increase in abdominal size and bloating as well as urinary symptoms.
The bottom line ladies: don't ignore your symptoms and tell your physician about your symptoms if they are persistent.
CA125 is a biomarker measured in the blood serum when we are monitoring ladies who have ovarian cancer. As a screening tool, however, CA125 is not good at all. It is not specific enough for ovarian cancer in that it may be elevated in other cancers, diseases or conditions.
What about imaging such as ultrasound?
It may play a better role in an enriched at risk population when used in conjunction with CA125. However, the interpretation of any abnormal scans may be more challenging in younger women leading to a higher rate of surgical interventions.
Furthermore, these ultrasounds are performed transvaginally, and therefore, overall relatively uncomfortable and borderline invasive. I don't know any woman who looks forward to a pelvic examination; therefore, compliance to annual transvaginal ultrasounds may be a challenge.
At this current time, in the absence of any effective screening, women are presenting with advanced ovarian cancer. Clinically, we see the enlarged abdomen, and by CT scan, we can see the tumor often has grown big enough to displace all other organs in the pelvis.
The current management for advanced ovarian cancer starts with surgical resection of the tumor. This is typically achieved through a laparotomy, which is a midline vertical skin incision made in the abdomen. The aim is to properly determine stage of the cancer and to remove all visible tumor. This in fact, may be a long surgery where it may take up to 8-10 hours.
By surgically removing the bulk of the tumor, it helps the chemotherapy given post-operatively work better. Furthermore, by removing the bulk of the tumor, you are in essence removing possible tumor cells that may be resistant to the chemotherapy. Importantly, by removing the tumor, patients are going to feel better with resolution of their symptoms as a result of having a large disease load debulked.
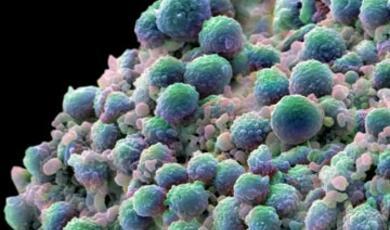
For the curious type in the audience wondering what is in this picture: this is the transverse colon that is highlighted with an omentum that has been replaced entirely by cancer. Ideally, you would like to preserve the bowel but in cases like this, it is not unusual to perform bowel resections with re-anastomosis, in order to remove all visible disease.
After surgery comes chemotherapy. I thought that I would take this opportunity to briefly discuss the history of chemotherapy and highlight the contributions of some of the pioneering physicians.
The first chemotherapy agent used was nitrogen mustard, which was used as a weapon during World War I. In 1946, Gilman and Goodman characterized their observation that when nitrogen mustard was given, there was profound lymphoid and myeloid suppression. They subsequently treated lymphomas with nitrogen mustard and received good results, although the patient's lymphoma came back after one month of remission.
Then in 1948, Farber used methotrexate which is a folic acid analogue in the treatment of acute lymphocytic leukemia. Folic acid is required for DNA synthesis, with an analogue, it stops DNA synthesis and the cell dies. This treatment was moderately successful; however, in those days, the results were perceived as quite astonishing. He published his findings in the New England Journal of Medicine, and was met with disbelief.
Just 10 years later in 1958, Roy Hertz and ChiuLi Min used methotrexate to treat choriocarcinoma which affects young women and is quite aggressive in that it starts in the trophoblastic tissues of a pregnancy and is often times metastasized to the liver, lungs and brain. Fortunately, it is also exquisitely chemosensitive. They were able to successfully treat choriocarcinoma with methotrexate. In fact, methotrexate remains the cornerstone in the treatment of the disease today.
In 1965, Holland, Freireich and Frei came up with the concept of multi-agent chemotherapy regimen to combat the issue of resistance. This was a radical idea at the time, especially given that supportive care was pretty much non-existent and the treatments had much toxicities.
Nevertheless, combination chemotherapy regimens are an important concept that we still use today in a majority of cancer types. In fact, we use a doublet chemotherapy regimen in ovarian cancer.
In ovarian cancer, as first line chemotherapy, we use carboplatinum and paclitaxel. After a major debulking surgery where we remove all visible tumor, we use chemotherapy to treat the microscopic disease that we can't see.
I would also like to point out that carboplatinum was a drug that was developed here in London at the Institute for Cancer Research. Paclitaxel is a drug that matured in the late 1980s and is a good example of a collaboration between the National Cancer Institute and a large pharmaceutical company, in this case Bristol Myers Squibbs.
Traditionally, these two drugs are highly emetogenic, meaning that they cause severe nausea and vomiting. Luckily, supportive medicine in cancer care has developed into a fully recognized subspecialty, and the medication we have to combat the side effects of chemotherapy is better than ever.
For patients with advanced ovarian cancer treated with surgery and chemotherapy, most will go into remission. Unfortunately, in most, the cancer comes back. The question then becomes what to treat, and this has to be answered with how long has it been since the last chemotherapy.
If the cancer comes back within 6 months, studies have shown that retreating with carboplatinum and paclitaxel will no longer be effective. If the time frame is longer than 6 months, these 2 drugs remain the treatment of choice.
Now, I would like to focus the remainder of my lecture on drug development in ovarian cancer in cases where the disease is no longer responsive to carboplatinum and paclitaxel.
There are a list of second line chemotherapy agents that we use in the States which offer perhaps a 15% efficacy rate. This is the reason why it is so important to develop new drugs. Ovarian cancer starts off as chemo-sensitive, but eventually, resistance becomes the issue to tackle.
We have witness the maturation of a new class of drugs, completely different from chemotherapy, in oncology. These are novel targeted agents. Through research, we have found certain proteins that are overexpressed in cancer which contribute to cancer's malignant features. And these new drugs target these over-expressed proteins. I will discuss briefly anti-angiogenic therapy, small molecule tyrosine kinase inhibitors, the biologics such as the monoclonal antibodies, and the recent success of the PARP inhibitors in ovarian cancer.
The principle of anti-angiogenic therapy lies within the fact that tumors, like all other organs in the body, need blood vessels to grow. In fact, as tumors start to outgrow its blood supply, it secretes important proteins that initiate the process of making new blood vessels.
One such protein is called VEGF, which stands for vascular endothelial growth factor.
This protein is particularly vital for tumor growth because it plays part in tumor proliferation, survival, migration and invasion
We now have different ways to combat the over-expression of VEGF. One of the methods is a monoclonal antibody against VEGF that quenches the circulating VEGF and nullifies its effects.
Perhaps you have heard of bevacizumab or its brand name Avastin which is made by Genetech in the States. 2007 was a big year for Avastin when it was initially approved by the FDA for the treatment of advanced colorectal cancer.
Subsequently it has been tested in chemo-resistant ovarian cancer, particularly in patients who have been treated with multiple different chemotherapies, and was found to have a response rate of 16%. And, this got all the gynecologic oncologists very excited at the drug's potential.
However, because the drug targets new blood vessels, and ovarian tumors grow on intestines, there was a high rate of intestinal perforation. Furthermore, for patients who have received more than 3 prior chemotherapy regimens, the perforation rate goes up to 24%.
Since then, we have learned that bevacizumab does have activity in ovarian cancer, and we can avoid intestinal perforation by carefully selecting our patients. Currently we have 2 large clinical trials on-going both here in the UK and in the US using this drug in ovarian cancer.
Another new class of drugs is known as tyrosine kinase inhibitors. On the surface of each cell, we have receptors for various proteins where the proteins make contact with the receptor and initiate a chain of signals within the cell.
Tyrosine kinase inhibitors are small molecules that target the receptor and stop the cascade of intracellular signalling. When such critical communication is intercepted, the cell is compromised.
There are many tyrosine kinase inhibitors under development. I should mention that one of the exciting stories for ovarian cancer is the evidence that PARP inhibitors have activity in BRCA-related ovarian cancer. PARP inhibitors are an example of a small molecule inhibitor.
PARP is a protein that binds to single strand breaks in the DNA and recruits other enzymes to fix and repair the broken DNA. Therefore, when PARP is inhibited, single strand base repair is prevented, leading to increased double strand breaks.
Now, if you recall, at the beginning of this lecture, I mentioned that BRCA mutation leads to impaired base repair. PARP inhibitors essentially cause a double-whammy to the genetically unstable cancer cells. This highlights the principle of synthetic lethality.
There are many other agents on the horizon for the treatment of ovarian cancer that target either the tumor cell or its supportive microenvironment.
We have seen activity in anti-angiogenics such a bevacizumab. Now there is a newer class of drug called VEGF-Trap that has been shown to be even more specific and potent in the preclinical setting.
Recent reports have also shown the clinical benefits of targeting folate receptors. In this category, perhaps the most developed is Morab003 which is now known as Farletuzumab. In 2008 at the American Society of Clinical Oncologists annual meeting, initial results from a clinical trial revealed that this drug, when used with conventional chemotherapy, has promising activity in relapsed ovarian cancer.
Targeting Her-2/Neu receptor is now part of standard care in patients with Her-2/Neu positive breast cancers. Again, targeting Her-2/Neu in ovarian cancer has had disappointing results.
Targeting CA125 certainly is logical, but trial data do not support its use in ovarian cancer at this time.
So, where do we go from here?
There are many pressing questions that we are in the midst of sorting out. First, is our current chemotherapy of carboplatin and paclitaxel the best option? Is there a better alternative with less toxicity? What if bevacizumab was added to the doublet-therapy right from the get-go? Can we prolong survival that way? These are all relevant questions, and there are massive multinational collaborative trials on-going to answer these questions.
Furthermore, if most patients with advanced ovarian cancer do experience a complete remission, is there anything that we can do to maintain their cancer free status? In this setting, what is a targeted therapy with a low toxicity profile that can get the job done?
And ultimately, we as oncologists want to see our patients as people living with cancer and not as people dying of cancer. Cancer should not be a terminal diagnosis. I believe that in our life time, we will see the day when cancer is being treated as a chronic disease, managed with close monitoring and treated with drugs that are well tolerated.
Although not yet part of routine cancer management, genomic analyses of tumor have the potential to drive a more individual specific care. In experimental setting, scientists have already determined tumor gene expression profiles that may assist in directing treatment options.
Back in 1975, if you were diagnosed with advanced ovarian cancer, your median survival was 12 months. Over the last 34 years, we have had major developments in chemotherapy and surgical techniques. Because of this, we have extended the median survival by almost 5-times.
However, there are areas that we should do better such as screening and treatment for recurrent disease. Certainly, these things are not easy, but I truly believe that we will get there in the next 10 years.I would like to thank you all for coming tonight.
In addition, I would like to thank my mentors from The University of Texas-MD Anderson Cancer Center, and the Royal Marsden here in London. The Fulbright Commission for giving me this opportunity to raise awareness and share my thoughts on ovarian cancer.
Also, my ovarian cancer patients who have been so supportive of my research, and who inspire me with their courage.
Most importantly, my family and friends- Thank you.
©Dr Liz Han, Gresham College
Part of:
This event was on Mon, 16 Nov 2009
Support Gresham
Gresham College has offered an outstanding education to the public free of charge for over 400 years. Today, Gresham College plays an important role in fostering a love of learning and a greater understanding of ourselves and the world around us. Your donation will help to widen our reach and to broaden our audience, allowing more people to benefit from a high-quality education from some of the brightest minds.


 Login
Login